
Prior Authorization for Certain Hospital OPD Services (Part A)
This option allows users to submit a prior authorization request (PAR) for certain hospital outpatient department (OPD) services. See Hospital Outpatient Department Prior Authorization for details about the prior authorization process.
NOTE: Since prior authorization is a condition of payment for the hospital OPD, this form is only available to users who sign in with a user ID registered to a Part A NPI/PTAN.
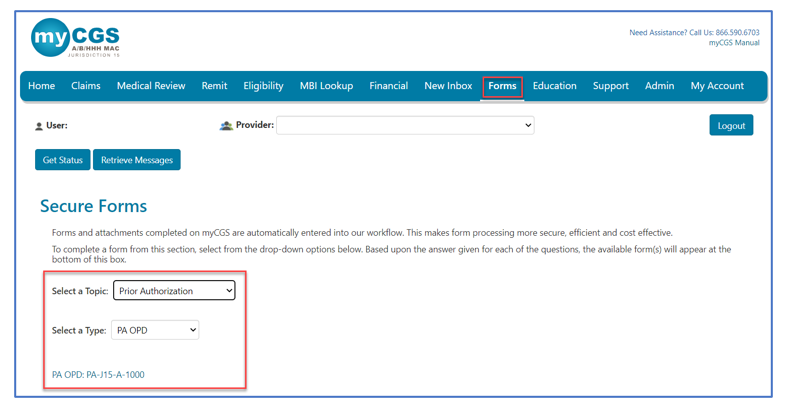
Once logged into myCGS, select the FORMS tab.
- Under the "Select a Topic" drop-down box, click "Prior Authorization."
- The "Select a Type" drop-down will default to "PA OPD."
- Select the "PA OPD: PA-J15-A-1000" link at the bottom of the page.
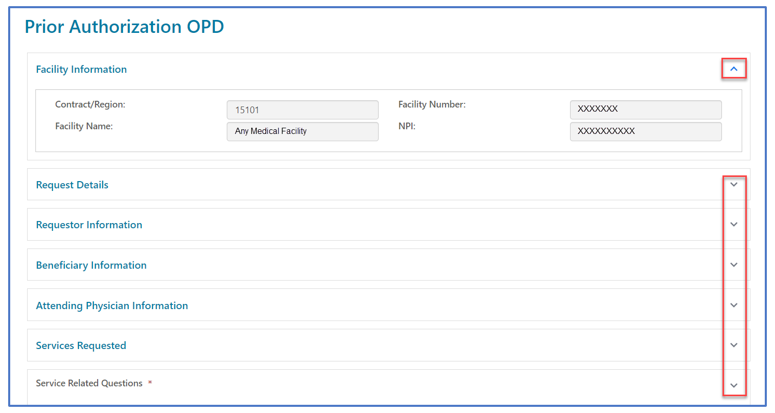
Once the PA form loads you will find several sections requiring your attention. Carrots at the top corners of each section allow you to collapse or expand the sections.
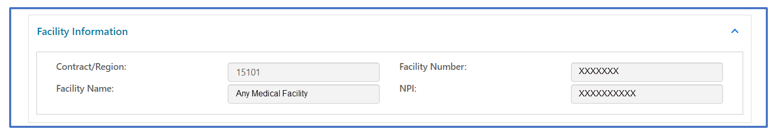
Facility Information
This section will auto-populate with information specific to your myCGS ID and provider information. No changes can be made to the Provider Information section.
Request Details
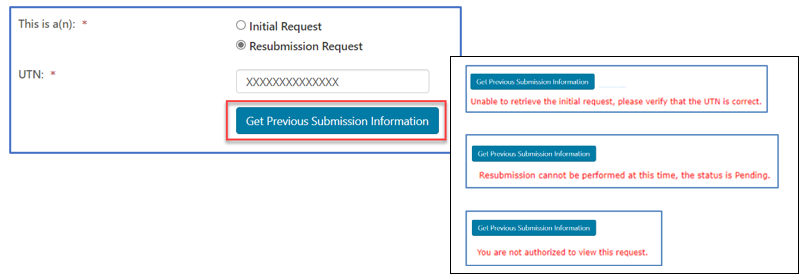
Select the appropriate request type.
- Initial Request: First prior authorization request (PAR) submission for this beneficiary/date of service.
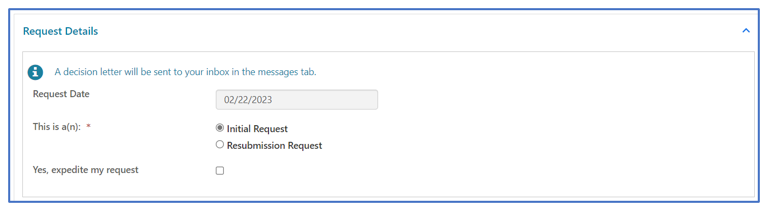
- Resubmission Request: Any subsequent PAR submission (i.e., to correct an error or omission identified after receiving a non-affirmation decision).
- Include additional/updated documentation not provided with a prior PAR.
- Enter the 14-digit unique tracking number (UTN) assigned to the most recent PAR. (Select 'Get Previous Submission Information' to verify).
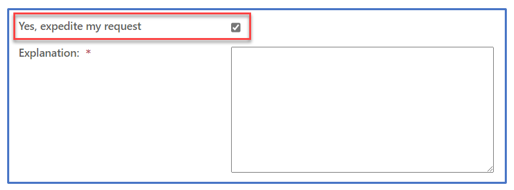
- Expedited Request: Used ONLY when a delay for a decision could seriously jeopardize the beneficiary's life, health or ability to regain maximum function. Enter the specific reason/rationale for CGS to substantiate the need for an expedited decision.
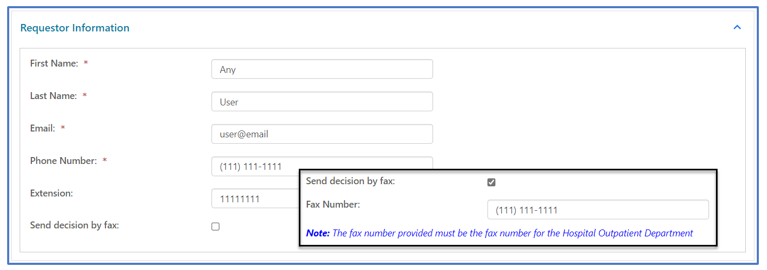
Requestor Information
This section identifies your name, email, and phone number associated with your myCGS user ID and will auto-populate. If you would like to receive your PAR decision via fax, check the box and enter the fax number of the hospital OPD.
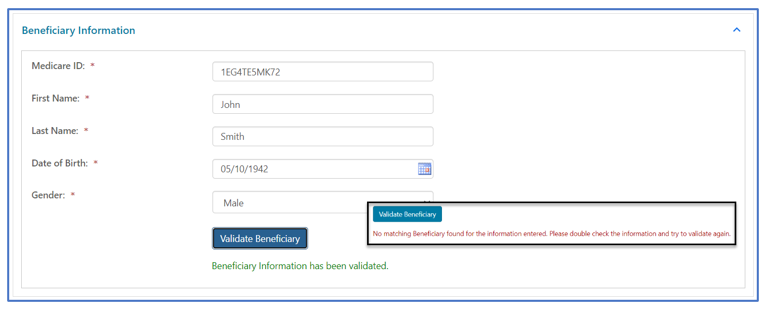
Beneficiary Information
Enter the beneficiary's Medicare ID, first name, last name, and date of birth.
For initial requests, select "Validate Beneficiary". myCGS will verify the information you entered corresponds with the beneficiary’s eligibility record on file.
NOTE: Refer to the beneficiary's Medicare card to verify this information before you submit a request.
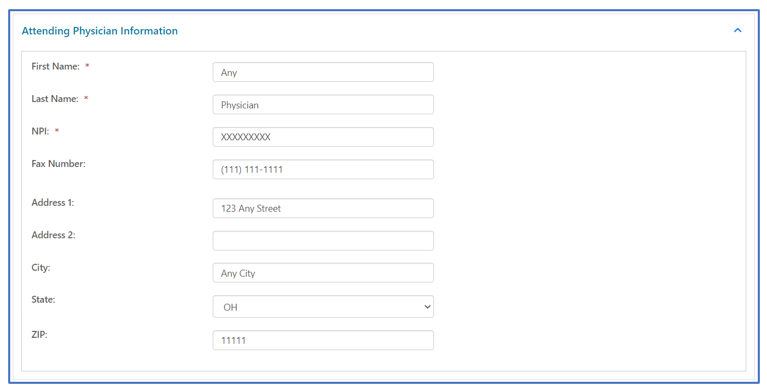
Attending Physician Information
Enter the name, National Provider Identifier (NPI), and complete address of the physician/non-physician practitioner (NPP) who has overall responsibility for the patient's medical care and treatment. If the attending physician would like to receive a copy of the PA decision letter, enter the physician's fax number to the form.
Services Requested
The "Services Requested" section of the form varies depending upon the type of service for the PAR.
- On the "Select a Service" drop-down, click on the service for which the PAR is for. Depending on the service selected, certain fields will display.
- HCPCS Code: Select the CPT code from the listing
- Primary Diagnosis Code: Enter the primary diagnosis code
- Number of Units: Enter the number of units (for Botulinum Toxin Injection PARs)
- Secondary Diagnosis Code: Identify a second diagnosis code, if applicable
- Related Codes: Enter any CPT/HCPCS codes related to those selected above
- Dates of Service: Enter the date the service will be rendered
- Type of Bill: Identify the appropriate TOB applicable to this service
- Part A hospital outpatient (TOB 13X)
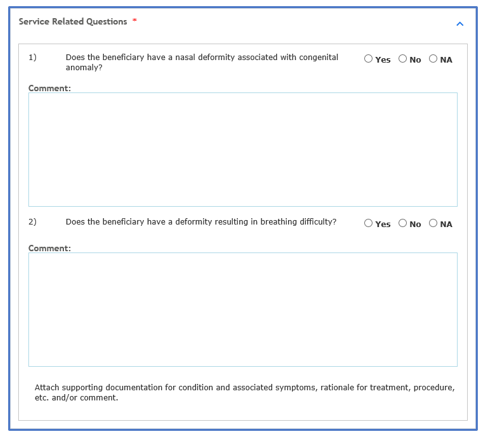
- Service Related Questions will display based upon the type of service. Answers to these questions help support medical necessity.
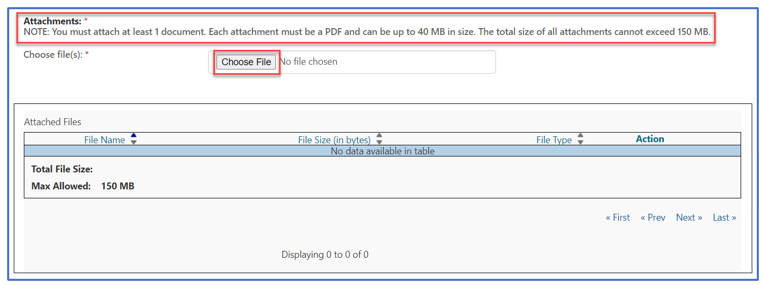
Attachments
Documentation from the medical record to support medical necessity of the service is to be attached to the myCGS form. Attachments must be in a PDF format and no large than 40MBs. The total of all attachments cannot exceed 150MBs.
NOTE: You must attach at least one document. Please refer to the applicable Local Coverage Determination and/or Local Coverage Article for direction.
Once the form is complete and all documentation attached, select "Submit" to send the PAR to CGS.
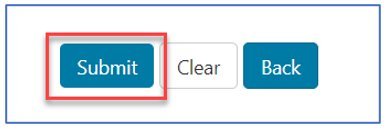
An eSignature box will display. Click OK to confirm the request and to sign the form.
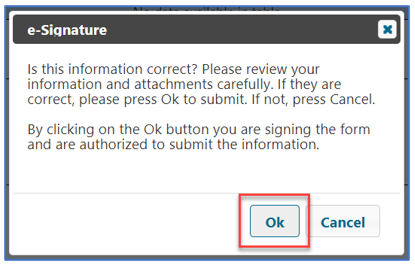
NOTE: If you do not click OK to sign the form, it will not be sent.
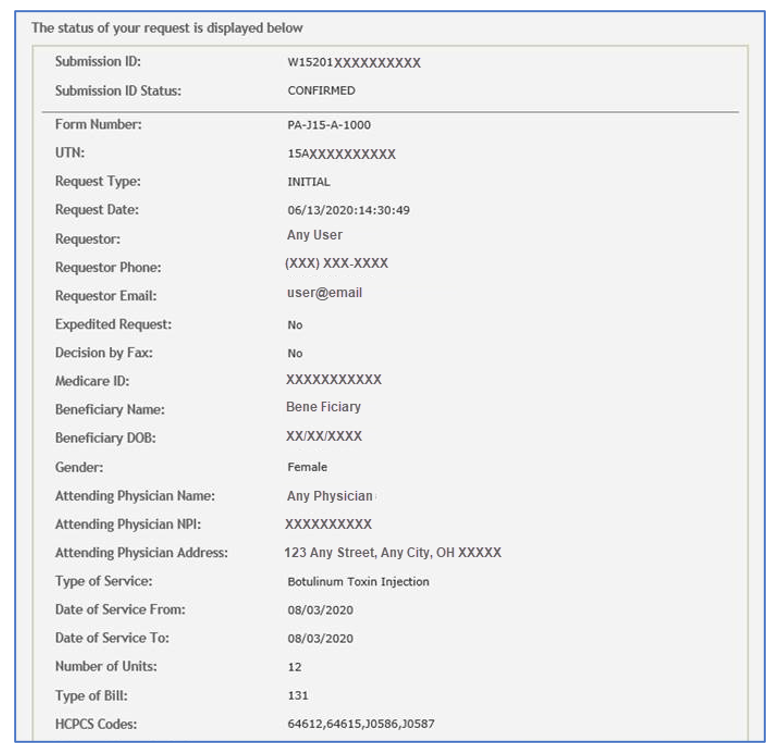
Confirmation
Confirmation messages will be delivered to your Messages inbox. The message that includes a Submission ID may be used to check the status of the PAR by entering the Submission ID into the "Get Status" screen located on any tab throughout the portal.
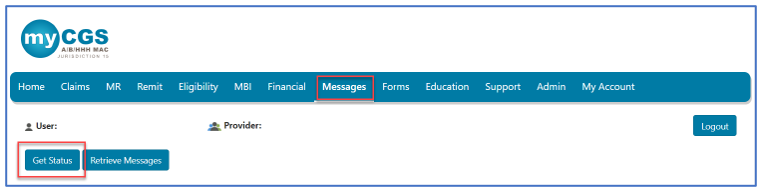
- PAR statuses available:
- Confirmed: CGS received the request.
- Decision: CGS issued an affirmed or non-affirmed decision. Refer to the PAR Decision Letter for details.
View PAR Decision Letter
The decision letters for PARs submitted through myCGS will be delivered to your myCGS Messages inbox (unless you request to receive it via Fax in the Requestor Information section above.) You may also check the Prior Authfolder for decision letters.
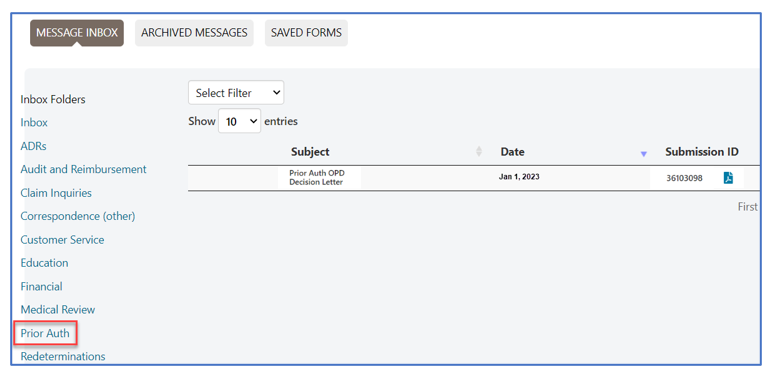
The decision letter will open as a PDF document.
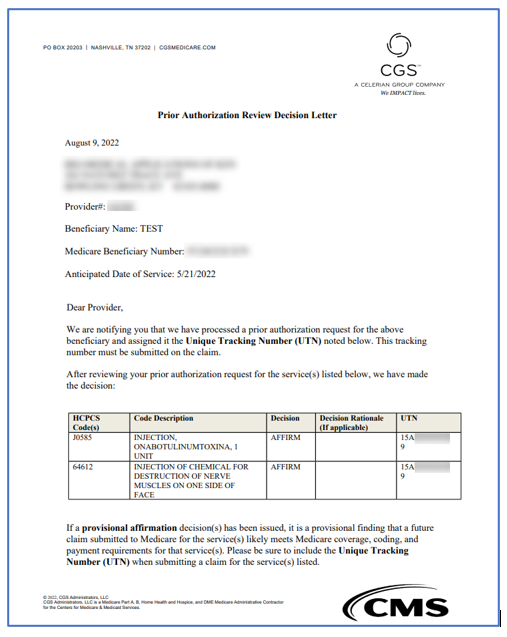
NOTE: PAR decisions and UTNs are valid for 120 days (the decision date is counted as day 1).


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn