
Audit & Reimbursement
Home Health, Hospice, and Part A providers are required to submit financial data, which support amounts claimed in a cost report, directly to CGS. This financial information is reviewed and processed by our Audit & Reimbursement (A&R) team.
This sensitive information and other correspondence may be submitted securely through myCGS.
NOTE: Per the Centers for Medicare & Medicaid Services (CMS), cost report submissions are no longer accepted through myCGS. Please refer to MLN Matters® article MM10611![]() for more on submitting cost reports.
for more on submitting cost reports.
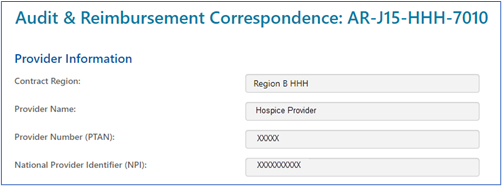
After clicking the “A&R Correspondence: AR-J15-HHH-7010” link and the form loads, the Provider Information section will auto-populate.
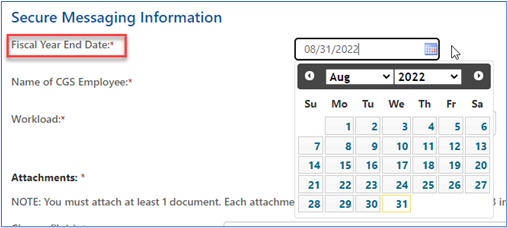
- From the 'Fiscal Year End Date' field, select the date from the calendar icon or enter the fiscal year end date in the XX/XX/XXXX format.
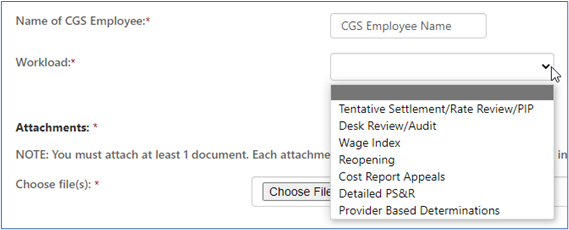
- Enter the name of the specific CGS employee for whom the correspondence is being sent.
- In the 'Workload' field, click the drop-down box to select the subject of your correspondence. The options available are:
- Tentative Settlement/Rate Review/PIP – Used to determine a tentative settlement after a cost report is submitted. A Rate Review and Periodic Interim Payment (PIP) are reviews to determine a rate to pay the provider.
- Desk Review/Audit – Reviews to determine the accuracy of the cost report for final settlement.
- Wage Index – A review of wages used by CMS to establish the wage index amounts used to calculate payment of claims.
- Reopening – A review of issue(s) from a cost report that has been previously settled. This review is subsequent to a request received by a provider to correct an error made during the desk review or audit, or based on new data not available to the provider prior to the submission of the original cost report.
- Cost Report Appeals – This is an appeal that may be requested that is related to adjustments made to the final settlement.
- Detailed PS&R – This is a listing of claims for a set period.
- Provider Based Determinations – A request to review provider based facilities to ensure they meet Medicare regulations.
NOTE: Please refer to MLN Matters® article MM10611![]() for more on submitting cost reports.
for more on submitting cost reports.
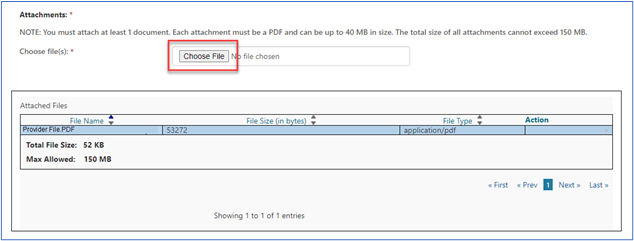
- You must upload at least one document to be sent with the form. Attachments can be up to 40MBs in size, not to exceed to total of 150MBs for all attachments. The documents must be in a PDF format.
- Click on the “Choose File” button and a window will open allowing you to locate and attach the PDF document to the form. Each attachment will populate in the “Attached Files” window.
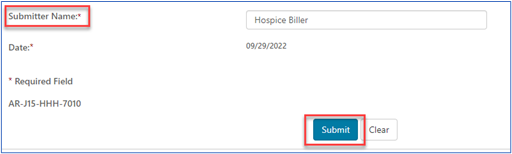
- Enter the name of the person submitting the form. Click the “Submit” button when the form is complete and ready to be submitted. The date will auto-populate.
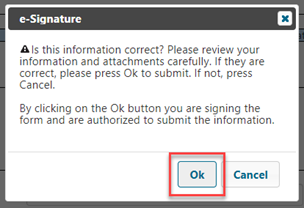
- An ‘e-signature’ box will appear, asking you to verify that the information entered and attachments are all correct. This ensures the signature requirements have been met.
Once received, confirmation will be delivered to your secure Messages inbox letting you know.
Responses sent to you from our A&R team will also be delivered to your Messages inbox.


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn