
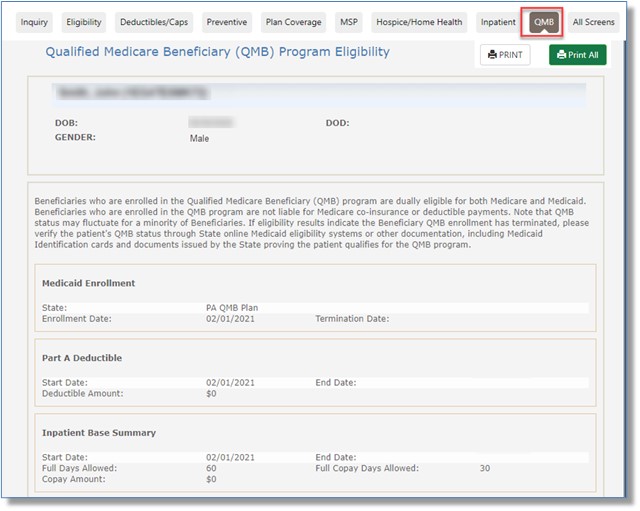
QMB
Beneficiaries who are enrolled in the Qualified Medicare Beneficiary (QMB) program are dually eligible for both Medicare and Medicaid. Those enrolled in this State Medicaid benefit, which assists low-income Medicare beneficiaries with Medicare Part A and Part B premiums and cost-sharing (deductibles, co-insurance/co-pays), are not liable financially.
QMB status may fluctuate for a minority of beneficiaries. If eligibility results indicate the beneficiary QMB enrollment has terminated, please verify the patient's QMB status through online State Medicaid eligibility systems or other documentation, including Medicaid identification cards and documents issued by the state proving the patient qualifies for the QMB program.
The "QMB" sub-tab includes Medicaid Enrollment, Part A Deductible, Inpatient, Skilled Nursing Facility (SNF), Part B Deductible, and Part B Co-Insurance sections.
NOTE: "$0" will display in the deductible, co-insurance, and co-pay sections for beneficiaries enrolled in the QMB program.


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn