myCGS User Manual

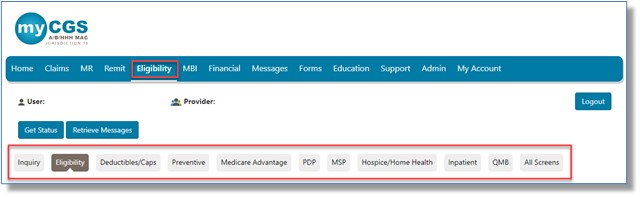
The myCGS eligibility function is based on CMS' HIPAA Eligibility Transaction System (HETS). When you choose the "Eligibility" tab, you will see a new set of sub-tabs with information related to your inquiry. Information is presented on the following:
|
|
|
|
|
|
|
|
|
|
NOTE: myCGS uses CMS' HETS 270/271 system, as required by CMS, for all eligibility inquiries. Although myCGS pulls data from HETS in real time, the data available in the HETS 270/271 system is updated only at certain times. CMS currently pulls the updated data Tuesday through Saturday during the hours of 6:00 p.m. - 8:00 p.m. This data is then uploaded into HETS during the hours of 9 p.m. to 6 a.m. As soon as updated data is available in the HETS 270/271 system, users will be able to view it in myCGS.
"Eligibility" Tab
To access beneficiary eligibility information, click on the "Eligibility" tab. Once selected, myCGS defaults to the "Inquiry" sub-tab.
Inquiry
Use the "Inquiry" sub-tab to enter beneficiary information to submit an eligibility request. To ensure accurate information is provided to you, all fields entered, including optional fields, must be an exact match to the data maintained in CMS' HETS.
The following combination of fields are required:
- Subscriber's Medicare ID, Last Name, and First Name, or
- Subscriber's Medicare ID, Last Name, and Date of Birth
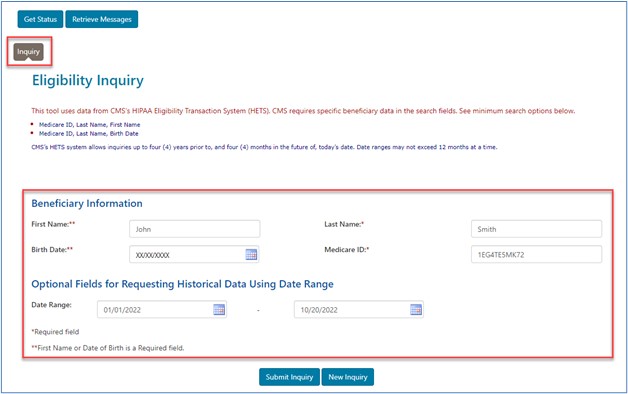
To ensure accurate historical data is returned, be sure to enter a date range in the Optional Fields area. You may enter dates up to four (4) years prior to, and four (4) months in the future of, the current date. Date ranges may not exceed 12 months at a time.
Click "Submit Inquiry" to obtain eligibility information. Once retrieved, all the other sub-tabs will populate with data related to that beneficiary and, if applicable, the date range entered.
For your convenience, you have the option of printing each individual sub-tab or the entire eligibility record.

Eligibility
The "Eligibility" sub-tab provides information regarding the beneficiary's Medicare coverage. If information does not populate, for example, either the "Part A Eligibility" or "Part B Eligibility" benefit information, it means the beneficiary is not eligible to receive Medicare benefits for the dates entered on the inquiry screen.
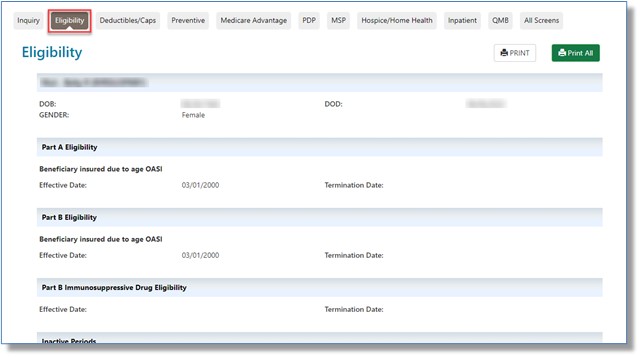
The following tables provide information for the "Eligibility" sub-tab fields:
Part A Eligibility Benefit Information
| Field Name | Description |
|---|---|
Effective Date |
The start of eligibility for Medicare Part A benefits. |
Termination Date |
The termination of eligibility for Medicare Part A benefits. No date in this field means Medicare Part A eligibility has not terminated. |
Part B Immunosuppressive Drug Eligibility
The Part B Immunosuppressive Drug (Part B-ID) benefit![]() is for patient who will lose End-Stage Renal Disease (ESRD) Medicare coverage 36 months after a kidney transplant and who don't have, and don't expect to have, certain other types of health care coverage. Starting January 1, 2023, this benefit will help continue to pay for immunosuppressive drugs.
is for patient who will lose End-Stage Renal Disease (ESRD) Medicare coverage 36 months after a kidney transplant and who don't have, and don't expect to have, certain other types of health care coverage. Starting January 1, 2023, this benefit will help continue to pay for immunosuppressive drugs.
myCGS will allow you to view Part B ID information for patients who are eligible.
| Field Name | Description |
|---|---|
Effective Date |
A date that indicates the start of Part B ID benefits |
Termination Date |
A date that indicates the end of Part B ID benefits |
Part B Eligibility Benefit Information
| Field Name | Description |
|---|---|
Effective Date |
The start of eligibility for Medicare Part B benefits |
Termination Date |
The termination of eligibility for Medicare Part B benefits. No date in this field means Medicare Part B eligibility has not terminated. |
Inactive Periods
| Field Name | Description |
|---|---|
Effective Date |
A date that indicates the start of an inactive period due to unlawful, deported, or incarcerated reasons |
Termination Date |
A date that indicates the end of an inactive period due to unlawful, deported, or incarcerated reasons |
Beneficiary Address
| Field Name | Description |
|---|---|
Address |
The address line 1 of the beneficiary |
Address 2 |
The address line 2 of the beneficiary, if available |
City |
The city of the beneficiary |
State |
The state of the beneficiary |
Zip |
The ZIP code of the beneficiary |
End Stage Renal Disease (ESRD) Information
| Field Name | Description |
|---|---|
Effective Date |
The date that indicates the start of eligibility for ESRD services |
End Date |
The date eligibility for ESRD services ended |
Dialysis Start Date |
The date the patient began dialysis |
Dialysis End Date |
The date dialysis ended for the patient |
Transplant Effective Date |
The date the patient received a transplant |
NOTE: The ESRD section displays only active ESRD data and will not be available if no notification has been received by CMS indicating an ESRD period is active and in effect per the date(s) requested.
MBI End Date
When a beneficiary's Medicare Beneficiary Identifier (MBI) is compromised, a new MBI is assigned and the previous is deactivated. The deactivation date will appear here.
Prior Authorization
Currently, certain hospital outpatient department (OPD) services and Repetitive Scheduled Non-Emergent Ambulance Transports (RSNAT) require prior authorization. If you need help determining whether a specific CPT/HCPCS code you bill requires prior authorization, check here for links to the Prior Authorization Decision Tree. Simply answer a series of YES/NO questions and this tool will help.
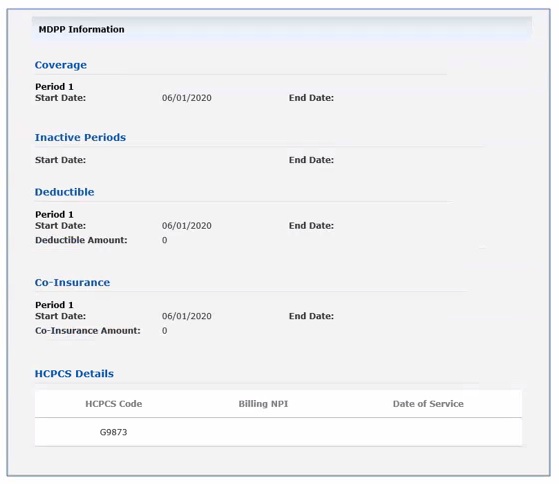
Medicare Diabetes Prevention Program (MDPP)
Patients who receive dedicated evidence-based services aimed to help prevent an indication of pre-diabetes from progressing to an onset of Type 2 diabetes will have information populated in this section, including coverage dates, HCPCS code G9873, the billing provider's National Provider Identifier (NPI), as well as specific dates of service.
Deductibles/Caps
The "Deductibles/Caps" sub-tab provides information regarding the beneficiary's Part B deductibles, co-insurance, occupational/physical/speech therapy caps, and other services.
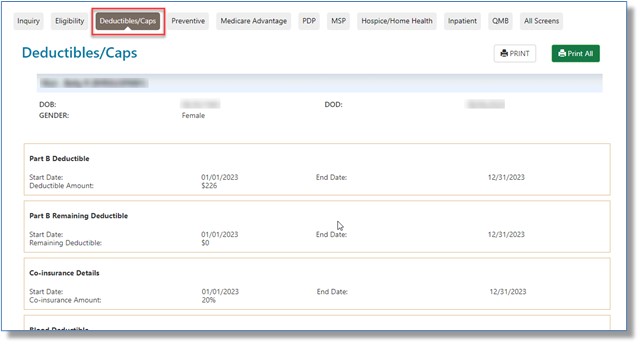
The following tables provide information for the "Deductible/Caps" sub-tab fields:
Part B Deductible
| Field Name | Description |
|---|---|
Start/End Date |
The beginning and end dates for the annual deductible |
Deductible Amount |
The Medicare Part B deductible amount associated with the calendar year |
Part B Remaining Deductible
| Field Name | Description |
|---|---|
Start/End Date |
The beginning and end dates for the annual deductible |
Remaining Deductible |
The Medicare Part B deductible amount remaining for the calendar year |
Co-insurance Details
| Field Name | Description |
|---|---|
Start/End Date |
The beginning and end dates for the annual co-insurance |
Co-insurance Amount |
The percentage of the patient's financial responsibility for Medicare Part B services |
Blood Deductible
| Field Name | Description |
|---|---|
Calendar Year |
The calendar year associated with the remaining deductible amount |
Number of Units Remaining |
The blood deductible units remaining associated with the calendar year indicated |
Occupational Therapy Cap
| Field Name | Description |
|---|---|
Calendar Year |
The calendar year associated with the capitation limit |
Amount Used |
The amount of allowed occupational therapy services applied |
Physical and Speech Therapy Cap
| Field Name | Description |
|---|---|
Calendar Year |
The calendar year associated with the capitation limit |
Remaining Amount |
The amount of allowed physical and speech-language pathology applied |
Pulmonary Rehabilitation Services
| Field Name | Description |
|---|---|
Calendar Year |
The calendar year associated with the pulmonary rehabilitation services |
Professional Sessions Remaining |
The number of pulmonary rehabilitation sessions remaining for the professional component |
Technical Sessions Remaining |
The number of pulmonary rehabilitation sessions remaining for the technical component |
Cardiac Rehabilitation Services
| Field Name | Description |
|---|---|
Calendar Year |
The calendar year associated with the cardiac rehabilitation services |
Professional Sessions Used |
The number of cardiac rehabilitation sessions used for the professional component |
Technical Sessions Used |
The number of cardiac rehabilitation sessions used for the technical component |
Intensive Cardiac Rehabilitation Services
| Field Name | Description |
|---|---|
Calendar Year |
The calendar year associated with the cardiac rehabilitation services |
Professional Sessions Used |
The number of intensive cardiac rehabilitation sessions used for the professional component |
Technical Sessions Used |
The number of intensive cardiac rehabilitation sessions used for the technical component |
Part B Free Services
| Field Name | Description |
|---|---|
STC Codes |
The Health Care Service Type Codes (STC) identify classifications of services or benefits. For definitions of the two-digit codes, view the link for "List of STC Codes." |
Value |
The patient's portion of responsibility for a benefit, represented as a percentage |
Start/End Date |
The start and end dates of the benefit period |
Mental Health Co-insurance
| Field Name | Description |
|---|---|
STC Codes |
The Health Care Service Type Codes (STC) identify classifications of services or benefits. For definitions of the two-digit codes, view the link for "List of STC Codes." This section is specific to mental health. |
Value |
The patient's portion of responsibility for a benefit, represented as a percentage |
Start/End Date |
The start and end dates of the benefit period, typically the first day of the calendar year indicated |
Preventive
The "Preventive" sub-tab provides information regarding preventive services the beneficiary has received.
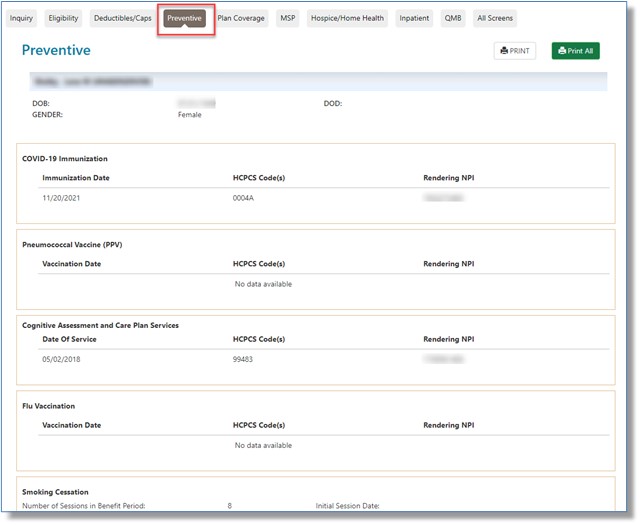
The following tables provide information for the "Preventive" sub-tab fields:
COVID-19 Immunization
myCGS will display the most recent information for the COVID-19 vaccines, boosters, and its administration.
| Field Name | Description |
|---|---|
Immunization Date |
The date the patient received the COVID vaccine/booster and/or administration of the vaccine. |
HCPCS Code |
Lists the specific vaccine/booster code the patient received and its corresponding administration code(s). |
Rendering NPI |
The National Provider Identifier (NPI) of the provider who rendered the vaccine/booster and its administration. |
Pneumococcal Vaccine (PPV)
This section identifies the dates of service the beneficiary received PPV (by CPT code) and the rendering provider's NPI.
| Field Name | Description |
|---|---|
Vaccination Date |
The date the patient received the PPV vaccine |
HCPCS Code |
Lists the specific code of the vaccine the patient received |
Rendering NPI |
The National Provider Identifier (NPI) of the provider who rendered the vaccine |
Cognitive Assessment and Care Plan Services
This section identifies if your patient received this service if signs of cognitive impairment were observed during a routine visit. Medicare covers a separate visit to assess your patient's cognitive function![]() and develop a care plan more thoroughly.
and develop a care plan more thoroughly.
| Field Name | Description |
|---|---|
Date of Service |
The date the patient received the service |
HCPCS Code |
Lists CPT code 99483, which is used to bill Cognitive Assessment & Care Plan Services |
Rendering NPI |
The National Provider Identifier (NPI) of the provider who rendered the service |
Flu Vaccination
You will find the patient's flu vaccination history in this section.
| Field Name | Description |
|---|---|
Vaccination Date |
The date the patient received a flu shot |
HCPCS Code |
Lists the specific code of the vaccine the patient received |
Rendering NPI |
The National Provider Identifier (NPI) of the provider who rendered the vaccine |
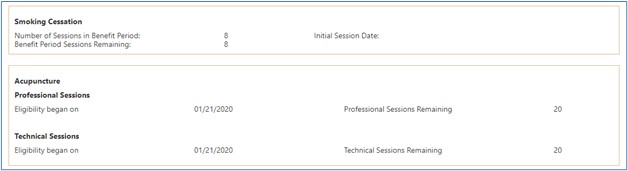
Smoking Cessation Information
Any smoker covered by Medicare is eligible to receive tobacco cessation counseling from a qualified physician/practitioner who can work with them to help them stop using tobacco.
| Field Name | Description |
|---|---|
Number of Sessions in Benefit Period |
Number of smoking cessation counseling sessions available for a beneficiary during the benefit period |
Initial Session Date |
The beginning date for smoking cessation counseling |
Benefit Period Sessions Remaining |
Number of smoking cessation counseling sessions remaining for a beneficiary |
Accupuncture
Effective for claims with dates of service (DOS) on and after January 21, 2020, Medicare will cover acupuncture for chronic Low Back Pain (cLBP)![]() .
.
| Field Name | Description |
|---|---|
Professional Sessions Eligibility date |
The date the patient began receiving professional acupuncture services. |
Professional Sessions Remaining |
The number of professional sessions the patient has left in the benefit period (out of a total of 20 sessions.) |
Technical Sessions Eligibility Date |
The date the patient began receiving professional acupuncture services. |
Technical Sessions Remaining |
The number of technical sessions the patient has left in the benefit period (out of a total of 20 sessions.) |
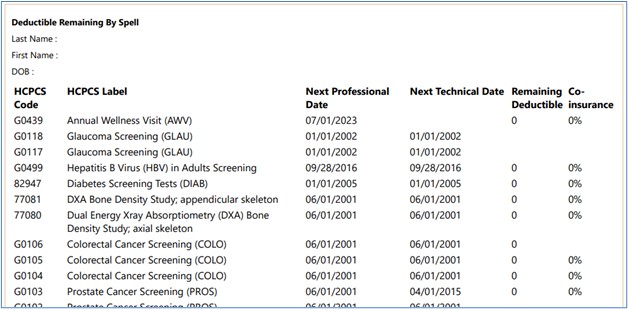
Deductible Remaining by Spell
This section identifies the Medicare-approved preventive services the beneficiary has received by CPT/HCPCS code and code description. Also, the dates the beneficiary is next eligible to receive services are listed as appropriate.
NOTE: Only HCPCS codes for which a beneficiary is eligible will be displayed and grouped together under their appropriate categories. If a service has been rendered, it is removed from the list until closer to the time the beneficiary is eligible to receive the service again.
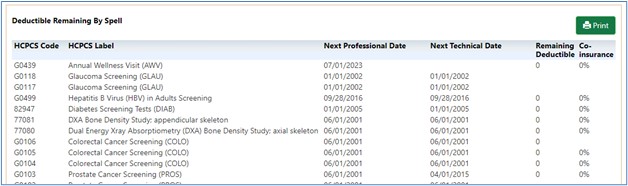
| Field Name | Description |
|---|---|
HCPCS Code |
The CPT or HCPCS code identifying the preventive service |
HCPCS Label |
A short descriptor of the CPT/HCPCS code identified in the first column |
Next Professional Date |
The date a beneficiary is next eligible for professional services associated with the indicated CPT/HCPCS code |
Next Technical Date |
The date a beneficiary is next eligible for technical services associated with the indicated CPT/HCPCS code |
Remaining Deductible |
The remaining deductible amount associated with the indicated CPT/HCPCS code |
Co-insurance |
The patient's portion of responsibility for the indicated CPT/HCPCS code, represented as a percentage |
Print Option
For a hardcopy record of the patient's preventive service history, click the Print icon. Doing this will generate a complete copy identifying the patient's name and date of birth in the header.
Medicare Advantage
The "Medicare Advantage" sub-tab provides information regarding the beneficiary's enrollment under Medicare Advantage (MA) Managed Care Plans (commonly referred to as Part C contracts) that provide Part A and B benefits for beneficiaries.
NOTE: Whenever myCGS indicates that a beneficiary has coverage through a non-Medicare entity (MA or Medicare Drug Benefit plans), the inquiring provider should always contact the non-Medicare entity for complete beneficiary entitlement information.
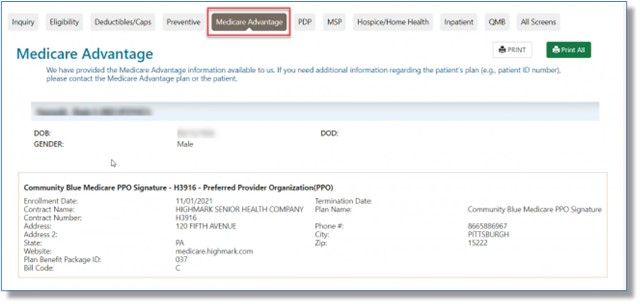
The table below describes the "Medicare Advantage" sub-tab fields:
| Field Name | Description |
|---|---|
Enrollment Date |
The date that indicates the start of enrollment to the coverage plan |
Termination Date |
The date that indicates the termination of enrollment to the coverage. No date in this field means the plan enrollment has not terminated. |
Contract Name |
A descriptive name of the beneficiary's insurance coverage organization |
Plan Name |
The name of the actual Medicare Advantage plan |
Contract Number |
The contract number (if on file) |
Address |
The coverage plan's address line 1 |
Phone Number |
The coverage plan's contract telephone number (if on file) |
Address 2 |
The coverage plan's address line 2 |
City |
The coverage plan's city |
State |
The coverage plan's state |
ZIP Code |
The coverage plan's ZIP code |
Website |
The coverage plan's website address that will provide information on the beneficiary's insurance |
Plan Benefit Package ID |
Identification number/code of the benefit package. |
Bill Code |
The bill code of the plan type. This field only applies to plan types HM, HN, IN, PR, and PS. Medicare Beneficiary "locked in" to MA Medicare Beneficiary NOT "locked in" to MA |
Prescription Drug Program (PDP)
The "PDP" sub-tab provides information on a beneficiary’s Part D prescription drug coverage.
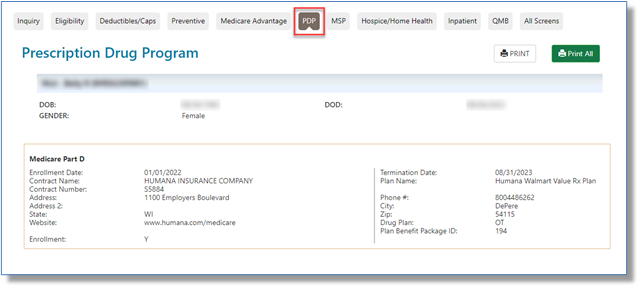
The table below describes the "PDP" sub-tab fields:
| Field Name | Description |
|---|---|
Enrollment Date |
The date that indicates the start of enrollment to the PDP. |
Termination Date |
The date that indicates the termination of enrollment to the PDP. No date in this field means the PDP enrollment has not terminated. |
Contract Name |
A descriptive name of the beneficiary's PDP coverage organization |
Plan Name |
The name of the actual PDP. |
Contract Number |
The contract number (if on file) |
Address |
The coverage plan's address line 1 |
Phone Number |
The coverage plan's contract telephone number (if on file) |
Address 2 |
The coverage plan's address line 2 |
City |
The coverage plan's city |
State |
The coverage plan's state |
ZIP Code |
The coverage plan's ZIP code |
Website |
The coverage plan's website address that will provide information on the beneficiary's insurance |
Drug Plan |
Code identifying the PCP |
Plan Benefit Package ID |
Identification number/code of the benefit package. |
MSP
The "MSP" sub-tab is populated if the beneficiary has a payer that process claims primary to Medicare. This sub-tab displays only active MSP data and will not be listed if there is no MSP data or if notification of coverage primary to Medicare has not been received by CMS.
NOTE: If a date range is entered on the "Inquiry" screen, it will affect the MSP data returned.
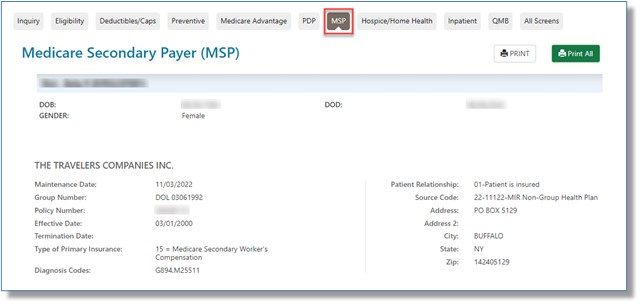
The table below describes the "MSP" sub-tab fields:
| Field Name | Description |
|---|---|
Maintenance Date |
The date maintenance was last performed on the record |
Patient Relationship |
Identifies if the patient is the actual insured |
Group Number |
Identifies the MSP Insurance Group Number or the MSP Date of Loss.
|
Policy Number |
The primary insuring organization's policy number for the Medicare beneficiary |
Effective Date |
The start date of the primary insurer's coverage |
Termination Date |
The termination date of the primary insurer's coverage. No date in this field means primary insurance coverage has not terminated. |
Type of Primary Insurance |
12 = Medicare Secondary – Working aged beneficiary or spouse with employer group health plan |
Diagnosis Codes |
Lists specific diagnosis codes associated with MSP insurance types, such as Workers' Compensation (WC), automobile, and liability situations. If the patient has MSP records based on diagnoses, the specific ICD-10 codes will display for your reference. |
Address |
The address line 1 of the insurance company |
Address 2 |
The address line 2 of the insurance company |
City |
The city of the insurance company |
State |
The state of the insurance company |
ZIP Code |
The ZIP code of the insurance company |
Hospice/Home Health
The Home Health Care section provides information for each episode start and end date and the corresponding billing activity dates.
The Hospice section provides eligibility information when the hospice benefit is effective and when it terminates, in addition to the total hospice occurrence count for the listed beneficiary.
If the patient has any gap in their episode of care or changes providers at any time, or if their hospice provider has sent the final claim revoking hospice care, you will see more than just a single effective date being returned. Once the final claim has been submitted, the hospice termination (or revocation) date is returned, along with the revocation code. If the patient is still in hospice care, but has changed providers, the start and termination date with each provider will be returned. Therefore, if no termination date is returned, it is to be assumed that the patient is still under hospice care, as no claim has yet been processed that revokes that period of care.
NOTE: The "Hospice/Home Health" sub-tab displays hospice and/or home health data and will not be accessible when there have been no claims received by CMS indicating hospice or home health coverage is active and is in effect per the date(s) requested. To make sure you see all the information, enter a date range in the inquiry screen.
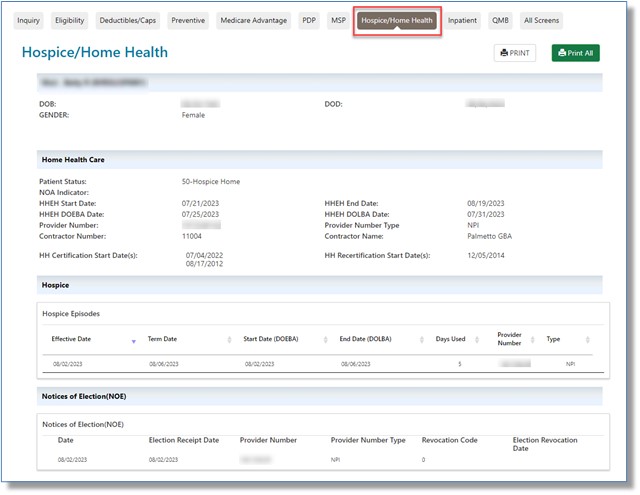
The tables below describe the "Home Health/Hospice" sub-tab fields:
Home Health Care
| Field Name | Description |
|---|---|
Patient Status |
Notes whether the patient is actively receiving services |
NOA Indicator |
Starting January 1, 2022, Medicare requires Home Health Agencies (HHAs) to submit a one-time Notice of Admission (NOA) instead of Requests for Anticipated Payment (RAPs). myCGS displays:
|
HHEH Start Date |
The date the 60-day home health episode period started |
HHEH End Date |
The date that the home health episode terminated |
HHEH DOEBA Date |
The date of earliest billing activity for spell of illness |
HHEH DOLBA Date |
The date of latest billing activity for spell of illness |
Provider Number |
The NPI of the home health facility |
Provider Number Type |
A display of "NPI" depending on the source of the provider number |
Contractor Number |
A display of the Medicare contractor number |
Contractor Name |
The name of the Medicare contractor |
HH Certification Start Date |
The date the beneficiary was certified to receive home health care services |
HH Recertification Start Date |
The date the beneficiary was recertified to continue receiving home health care services |
Hospice
| Field Name | Description |
|---|---|
Effective Date |
The start date of a beneficiary's elected period of hospice coverage |
Term Date |
The termination date of a beneficiary's elected period of hospice coverage. No date in this field means the beneficiary's elected period of hospice coverage has not terminated. |
Start Date (DOEBA) |
Date of Earliest Billing Activity |
End Date (DOLBA) |
Date of Latest Billing Activity |
Days Used |
The number of Hospice days used |
Provider Number |
The NPI of the hospice facility |
Type |
A display of "NPI" as the type of provider number |
Notices of Election (NOE) |
The Notice of Election (NOE) is to be submitted within 5 days after a hospice admission in order to be considered timely.
|
Revocation Code |
The code indicating the revocation status for the spell listed Medicare Beneficiary in Hospice Care Medicare Beneficiary with Hospice Care Revoked |
Election Revocation Date |
The date the spell revoked |
myCGS will display up to 50 billed Hospice episodes that occurred in the last four years.
Inpatient
The "Inpatient" sub-tab includes Inpatient, Skilled Nursing Facility (SNF), and Psychiatric Benefit Data sections. The Inpatient section provides hospital inpatient benefit and billing information. The SNF section provides SNF benefit and billing information.
NOTE: While the Psychiatric Benefit Data section now displays in myCGS, the data is not yet available in CMS' HIPAA Eligibility Transaction System (HETS) 270/271 system that we are required to access for eligibility.
The system will return hospital inpatient default deductibles based on the requested start year when the following occurs:
- No inpatient spell data returned from the database overlaps or falls within 60 days of the requested date (range)
- Entitlement period and request date period overlap
- Part A entitlement start year is less than the requested start year
In addition, the system will continue to return the hospital inpatient default deductible remaining amounts, inpatient co-payment days, and SNF co-payment days based on the beneficiary's Part A entitlement start year when the following occurs:
- No inpatient spell data returned from the database overlaps or falls within 60 days of the requested date (range)
- Entitlement period and request date period overlap
- Part A entitlement start year is less than or equal to the requested start year
NOTE: Depending on the date(s) range requested, multiple inpatient and SNF spells might be displayed. The data returned on this screen is directly impacted by timely submission of claims by the provider. The data returned is compiled from claims that have been processed by the Common Working File (CWF). To make sure you see all the information, enter a date range in the inquiry screen.
If a single hospital inpatient/SNF spell spans more than one calendar year, myCGS will return the daily co-payment amounts associated with the beginning year of the spell.
If there is no hospital inpatient/SNF spell within 60 days of the requested date(s) of service, myCGS will return default values for Part A spell data.
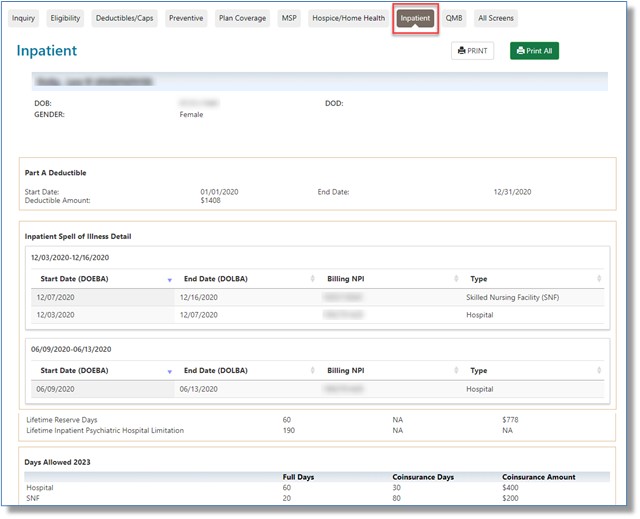
The table below describes the "Inpatient" sub-tab fields:
Part A Deductible
| Field Name | Description |
|---|---|
Start/End Date |
The beginning and end date for the calendar year requested. |
Deductible Amount |
The Medicare Part A deductible amount applied to each spell of illness that occurs during the calendar year. |
Inpatient Spell of Illness Detail
| Field Name | Description |
|---|---|
Start Date (DOEBA) |
The date of earliest billing activity for the spell of illness |
End Date (DOLBA) |
The date of latest billing activity for the spell of illness |
Billing NPI |
The billing NPI of the hospital and/or SNF. You may refer to the NPPES NPI Registry |
Type |
Displays the type of provider identified in the Billing NPI field |
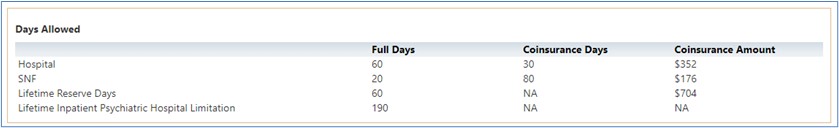
Days Allowed
Identifies the number full and co-insurance days allowed for hospital, skilled nursing facility (SNF), Lifetime Reserve, and Lifetime Inpatient Psychiatric Hospital based upon the calendar year requested. The co-insurance amounts are displayed for each, as well.
Days Remaining
| Field Name | Description |
|---|---|
DOEBA |
The date of earliest billing activity for the spell of illness |
DOLBA |
The date of latest billing activity for the spell of illness |
Full Days |
The number of inpatient full days allowed for the calendar year requested |
Co-insurance Days |
The number of inpatient full co-insurance days allowed for the calendar year requested |
Billing NPI |
The billing NPI of the hospital and/or SNF. You may refer to the NPPES NPI Registry to find the facility’s contact information. |
Part A Free Services
| Field Name | Description |
|---|---|
STC Codes |
The Health Care Service Type Codes (STC) identify classifications of services or benefits. For definitions of the two-digit codes, view the link for "List of STC Codes." |
Value |
The patient's portion of responsibility for a benefit, represented as a percentage |
Start/End Date |
The start and end dates of the benefit period |
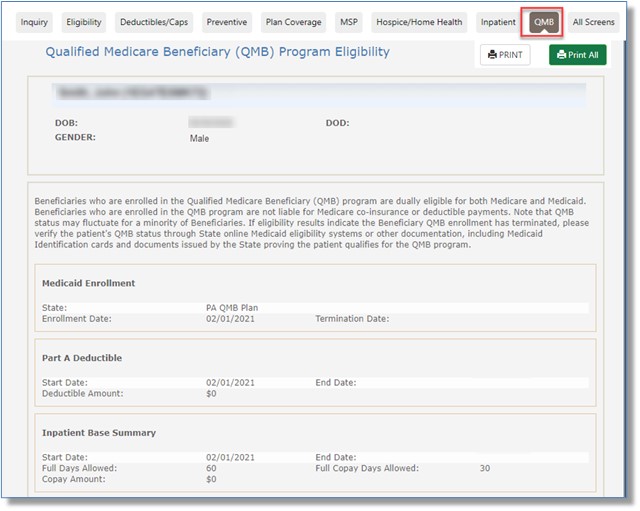
QMB
Beneficiaries who are enrolled in the Qualified Medicare Beneficiary (QMB) program are dually eligible for both Medicare and Medicaid. Those enrolled in this State Medicaid benefit, which assists low-income Medicare beneficiaries with Medicare Part A and Part B premiums and cost-sharing (deductibles, co-insurance/co-pays), are not liable financially.
QMB status may fluctuate for a minority of beneficiaries. If eligibility results indicate the beneficiary QMB enrollment has terminated, please verify the patient's QMB status through online State Medicaid eligibility systems or other documentation, including Medicaid identification cards and documents issued by the state proving the patient qualifies for the QMB program.
The "QMB" sub-tab includes Medicaid Enrollment, Part A Deductible, Inpatient, Skilled Nursing Facility (SNF), Part B Deductible, and Part B Co-Insurance sections.
NOTE: "$0" will display in the deductible, co-insurance, and co-pay sections for beneficiaries enrolled in the QMB program.
All Screens
For your convenience, this sub-tab combines all of the information from the other sub-tabs, allowing you to scroll through the data much faster.



 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn