
Medicare Secondary Payer (MSP) Claim
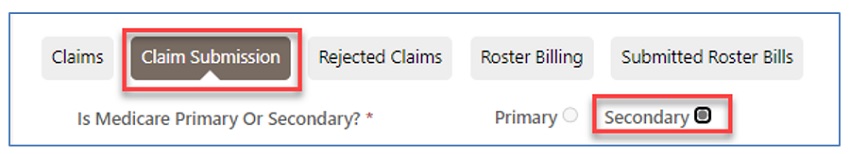
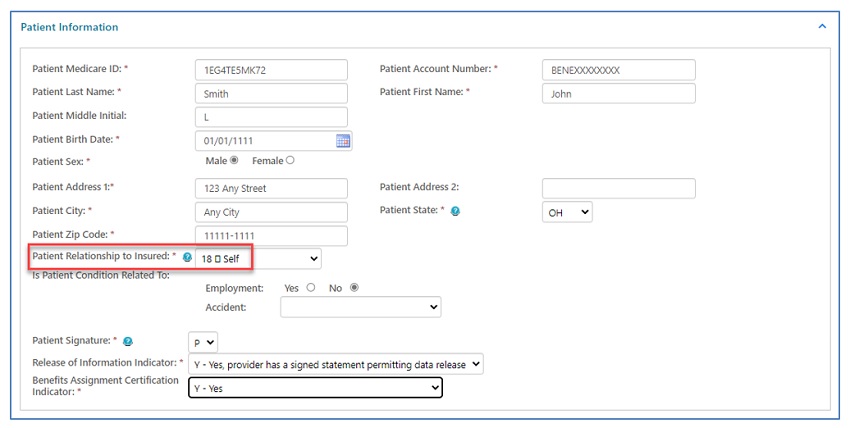
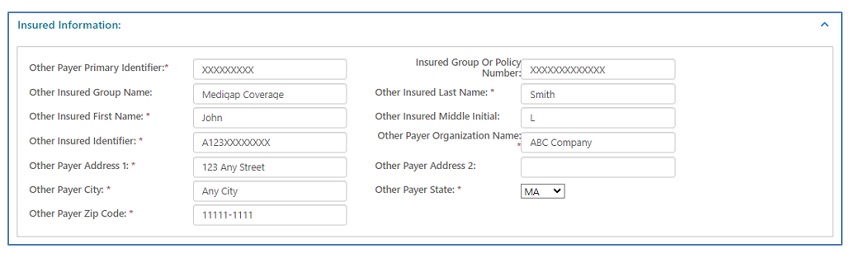
When "Secondary" is selected at the top of the claim, the form will display a "Patient Relationship to Insured" field and "Insured Information" section located further down.
Under "Miscellaneous Claim Information," additional fields will display. Be sure to identify the Insurance Type Code.
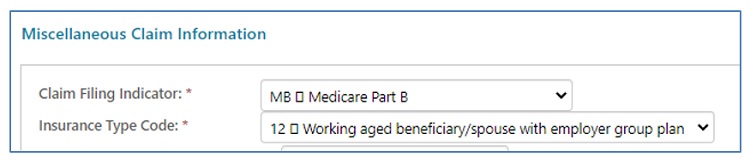
NOTE: Refer to the Eligibility/MSP section of this user manual to locate the Insurance Type.
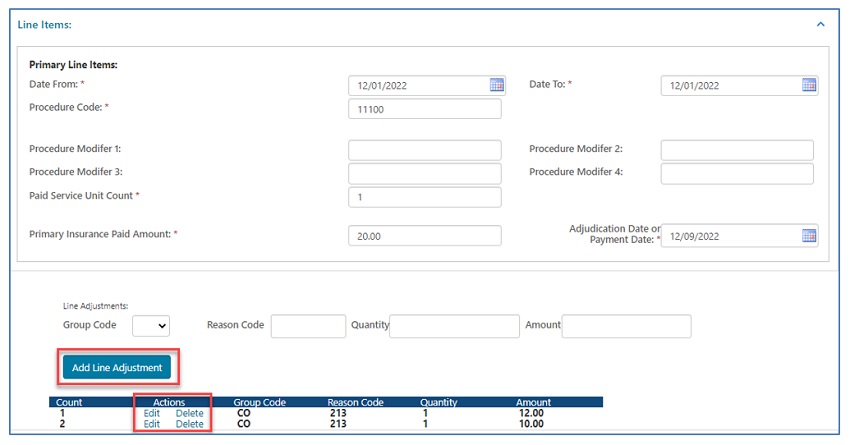
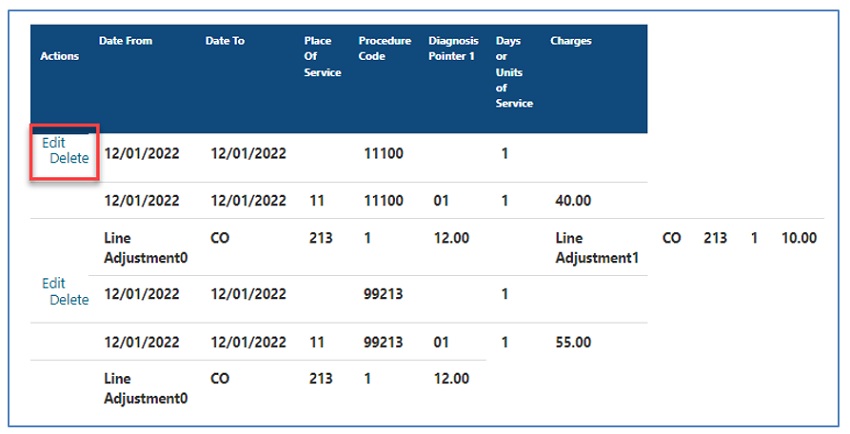
- Enter line items individually.
- MSP claims will display "Primary Insurance Paid Amount" and "Adjudication or Payment Date" fields.
- Reason/remark codes from the primary insurance explanation of benefits (EOB) are required in the "Line Adjustments" fields.
- Click "Add Line Adjustments" after entering each line item.
- Select "Edit" to make changes or "Delete" to remove line items.
- Under "Secondary Line Items," the date, procedure code, modifier, and units fields will auto-populate based on the data entered above.
- Complete the place of service, diagnosis pointer, charge, and other applicable fields.
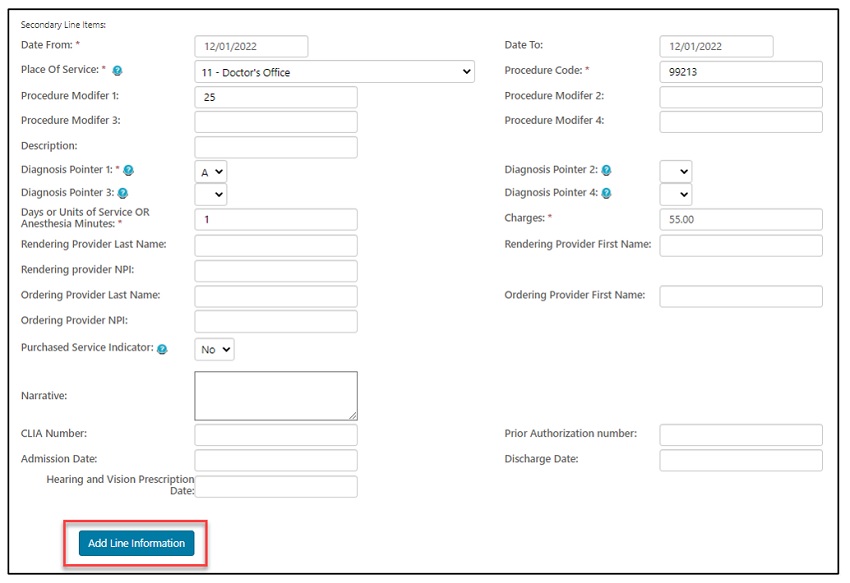
- Click "Add Line Information" after entering each line item.
- Select "Edit" to make changes or "Delete" to remove line items.
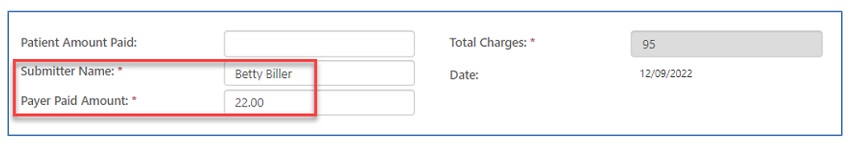
- Enter the "Patient Amount Paid" ONLY when the patient paid for the service prior to submitting the claim.
- Enter the name of the person authorized to submit the claim on behalf of the provider. This will serve as an electronic signature.
- Also enter the amount paid by the primary insurance.
NOTE: The primary insurance EOB is NOT required. Include any attachments needed to support allowing the service(s) submitted.


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn