
Redeterminations
Providers and beneficiaries may appeal an initial claim determination when Medicare's decision is to deny or partially deny a claim. The first level of the appeal process is Redetermination. You have 120 days from the date of receipt of the notice of initial determination to submit a request. There is no monetary threshold.
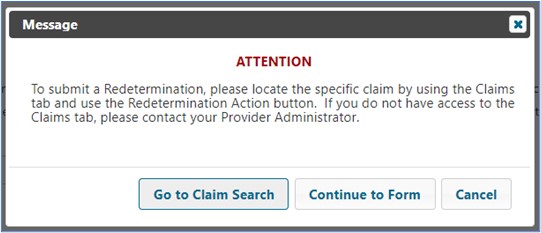
Note: Access this form from the Claims tab to ensure the form correctly auto-populates with the information we need to process your request.
Refer to the Appeals section of this manual for step-by-step instructions on how to complete and submit Redeterminations.


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn