
Claim Status
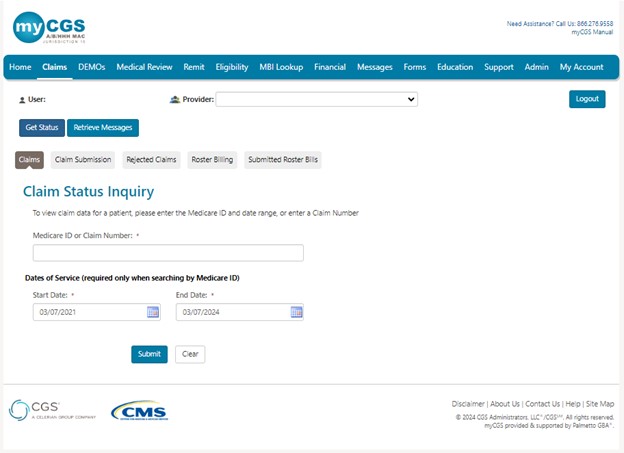
To access claim information:
- Select the "Claims"tab. The "Claim Status Inquiry" page will display.
- You can now enter either the MBI or Internal/Document Control Number (ICN/DCN) in the field.
- The date of service will be pre-populated with the last three years and is editable. Enter a date of service in the MM/DD/CCYY format or select the calendar icon
 to select the date.
to select the date. - Please note, there will be times when the original ICN/DCN of the claim will not display. An example of this is when the claim has been adjusted, in which case the adjustment number will display instead. Please search using the MBI option.
NOTE: Retrieving claims information older than 6 months may take additional time. In addition, offline claims will not be displayed. Many claims are offline after 3 years, sometimes earlier.
- The date of service will be pre-populated with the last three years and is editable. Enter a date of service in the MM/DD/CCYY format or select the calendar icon
- Click Submit.
Claims that are paid, in process, returned or denied are displayed. Information is retrieved from CMS standard systems and is as current as the standard systems. Claims that are offline or returned without processing will not appear. Nor will the original ICN/DCN of claims that have been adjusted.
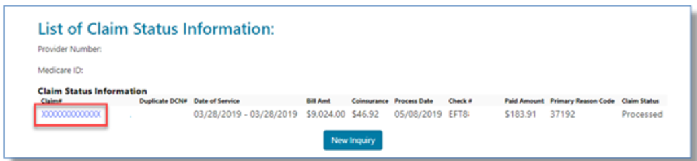
If finalized, information specific to the claim will display such as ICN/DCN, duplicate DCN (if applicable for A/HHH claims), date of service, billed amount, co-insurance amount, date processed, check number, amount paid, reason code (A/HHH), and general status.


 Join Electronic Mailing List
Join Electronic Mailing List Print
Print Bookmark
Bookmark Email
Email Facebook
Facebook YouTube
YouTube LinkedIn
LinkedIn