Claim Denials
There are a variety of reasons your claim may have denied. While we can't provide you with every possible scenario, we can help you interpret the American National Standards Institute (ANSI) Reason Codes![]() referenced on your Remittance Advice.
referenced on your Remittance Advice.
In some cases, you can simply correct and resubmit your claim for processing and payment consideration. For more complex issues, you may need to request a Reopening or a Redetermination.
If you see frequent denials, we recommend you consider participating in one of our education workshops/seminars, Webinars, or review the variety of online education available.
CGS Wizard
CGS Wizard contains processed claim details for all claims submitted to Jurisdiction C, ADR status, medical review decisions and resources directly from our website! Just enter a 14-digit CCN (claim control number) and CGS Wizard will give you the claim and/or medical review denial details you need to resubmit your claim!
Claim Denial Resolution Tool
This tool has been developed to provide the supplier community guidance on how to address claim denials in the most efficient manner. Enter the ANSI Reason Code from your Remittance Advice into the search field below. The tool will provide the remittance message for the denial and the possible causes and resolution. Please Note: This tool is available for claim denial assistance with the common denials and may not address every scenario.
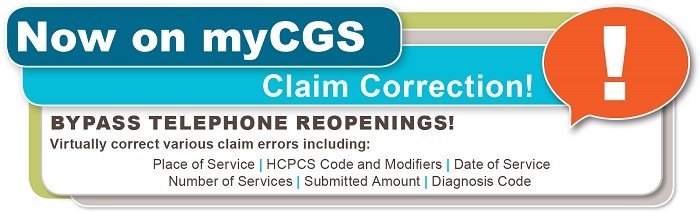
myCGS Web Portal
The myCGS Web Portal offers the ability to correct claim errors. To get started, refer to the myCGS Registration and Account Management Guide for detailed instructions on how to register.
Related Information |
Related EducationEducación en Español |
Updated: 02.17.2026