April 9, 2024
Documentation Guidelines for Evaluation & Management (E/M) Services: Reminders and Updates
The Centers for Medicare & Medicaid Services (CMS) and the American Medical Association (AMA) developed Evaluation & Management Documentation Guidelines to assist health care providers that submit claims to Medicare in documenting and correctly coding E/M services. There are two sets of guidelines, commonly known as the 1995 guidelines and 1997 guidelines. The following information was extracted from these guidelines and is a reminder about the intent of and principles behind documentation in patients' medical records.
Medical Necessity
Services rendered should be billed to Medicare based on the medical necessity of the visit. If the visit does not necessitate the detail of documentation required to meet the CPT® code, a lower level of service should be billed. Do not include additional components in the record for the sole purpose of meeting a specific CPT® code.
"Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT® code. It would not be medically necessary or appropriate to bill a higher level of evaluation and management service when a lower level of service is warranted. The volume of documentation should not be the primary influence upon which a specific level of service is billed. Documentation should support the level of service reported."
Reference: CMS Medicare Claims Processing Manual (Pub. 100-04), chapter 12, section 30.6.1![]()
Documentation Principles
Clear and concise medical record documentation is critical to giving patients quality care and getting correct and prompt payment for services. Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history, including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record should clearly and concisely document the evaluation and plan of the patient's immediate treatment as well as chronologically track the patient's care over time.
An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary.
Documentation is required to make sure a service is consistent and to confirm:
- Site of service
- Medical necessity and appropriateness of diagnostic or therapeutic services
- Services are reported correctly
The documentation principles listed below apply to all types of medical and surgical services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. The general principles listed below may be modified to account for these variable circumstances in providing E/M services.
- The medical record should be complete and legible.
- The documentation of each patient encounter may include:
- reason for the encounter and relevant history;
- physical examination findings and prior diagnostic test results;
- assessment, clinical impression, or diagnosis;
- rationale for ordering diagnostic and other ancillary services;
- plan for care; and
- date of the service and legible identity of the observer.
- Past and present diagnoses should be accessible to the treating and/or consulting physician.
- Appropriate health risk factors should be identified.
- The patient's progress, response to and changes in treatment, and revision of diagnosis should be documented.
- The CPT and ICD-10-CM codes reported on the health insurance claim form or billing statement should be supported by the documentation in the medical record.
UPDATES
Effective January 1, 2023, the AMA CPT Editorial Panel approved revised coding and updated guidelines for "Other E/M visits" (which includes hospital inpatient, hospital observation, emergency department, nursing facility, home or residence services, and cognitive impairment assessments). CMS is adopting most of the CPT's revised guidance, including deletion of several CPT codes.
The E/M code and guideline changes are like those already applied to office and other outpatient visits, which were effective for dates of service on and after January 1, 2021.
Practitioners will no longer use history and exam to select the office/outpatient E/M visit level. Instead, an office/outpatient E/M visit includes a medically appropriate history and exam, when performed. Practitioners should perform history and exam to the extent clinically appropriate, and reasonable and necessary.
Effective for dates of service (DOS) on and after January 1, 2023, practitioners have the choice to document most E/M visits via medical decision making (MDM) or time, except emergency department visits and cognitive impairment assessments, which are not timed services.
Guidelines for Selecting Level of Service Based on Medical Decision Making
Four types of MDM are recognized: straightforward, low, moderate, and high. The concept of the level of MDM does not apply to 99211, 99281.
MDM includes establishing diagnoses, assessing the status of a condition, and/or selecting a management option. MDM is defined by three elements:
- The number and complexity of problem(s) that are addressed during the encounter.
- The amount and/or complexity of data to be reviewed and analyzed. These data include medical records, tests, and/or other information that must be obtained, ordered, reviewed, and analyzed for the encounter. This includes information obtained from multiple sources or interprofessional communications that are not reported separately and interpretation of tests that are not reported separately.
- The risk of complications and/or morbidity or mortality of patient management. This includes decisions made at the encounter associated with diagnostic procedure(s) and treatment(s). This includes the possible management options selected and those considered but not selected after shared decision making with the patient and/or family. Shared decision making involves eliciting patient and/or family preferences, patient and/or family education, and explaining risks and benefits of management options.
Guidelines for Selecting Level of Service Based on Time
For coding purposes, time for these services is the total time on the date of the encounter. It includes both the face-to-face time with the patient and/or family/caregiver and non-face-to-face time personally spent by the physician and/or other qualified health care professional(s) on the day of the encounter (includes time in activities that require the physician or other qualified health care professional and does not include time in activities normally performed by clinical staff). It includes time regardless of the location of the physician or other qualified health care professional (e.g., whether on or off the inpatient unit or in or out of the outpatient office). It does not include any time spent in the performance of other separately reported service(s).
A shared or split visit is defined as a visit in which a physician and other qualified health care professional(s) both provide the face-to-face and non-face-to-face work related to the visit. When time is being used to select the appropriate level of services for which time-based reporting of shared or split visits is allowed, the time personally spent by the physician and other qualified health care professional(s) assessing and managing the patient and/or counseling, educating, communicating results to the patient/family/caregiver on the date of the encounter is summed to define total time.
Physician or other qualified health care professional time includes the following activities, when performed:
- preparing to see the patient (e.g., review of tests)
- obtaining and/or reviewing separately obtained history
- performing a medically appropriate examination and/or evaluation
- counseling and educating the patient/family/caregiver
- ordering medications, tests, or procedures
- referring and communicating with other health care professionals (when not separately reported)
- documenting clinical information in the electronic or other health record
- independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver
- care coordination (not separately reported)
Do not count time spent on the following:
- the performance of other services that are reported separately
- travel
- teaching that is general and not limited to discussion that is required for the management of a specific patient
Note: Time alone does not determine the level of service. Documentation must support the level of service billed.
Signature and Record Keeping Reminders from CGS
All documentation should include the name, signature and credentials of the person performing the service.
- Signature and credentials of person performing the service meet CMS signature requirements for timeliness (should be signed same day of visit)
- Amendments/corrections/delayed entries are properly identified.
- Amendments/corrections/delayed entries are initialed and dated by Author within 30 days of the billed service.
Response to Additional Documentation Requests (ADRs) should include but not limited to:
- Physician's progress notes
- Initial history and physical
- Physician's orders
- Procedure notes
- Assessment, clinical impression, or diagnosis
- X-ray, diagnostic test, and laboratory results
- Medical plan of care
- Any additional documentation verifying medical necessity
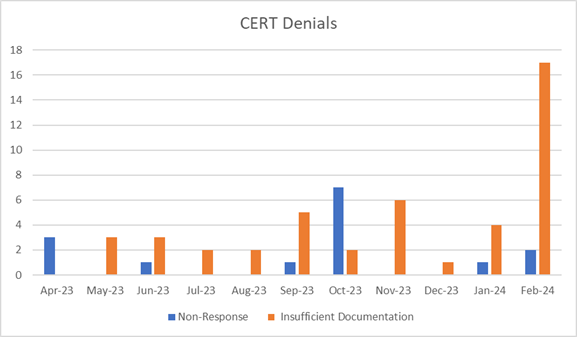
CERT identified errors in E/M services
Reviewers determine claims have errors when the medical documentation submitted is insufficient to support Medicare payment for the services billed (that is, the reviewer couldn't conclude some of the allowed services were provided, were provided at the level billed, or were medically necessary).
High errors consisted of insufficient documentation, medical necessity, and incorrect coding of E/M services to support medical necessity and accurate billing of those services.
Specific errors identified:
Additional Resources
- 1995 Documentation Guidelines for Evaluation and Management Services

- 1997 Documentation Guidelines for Evaluation and Management Services

- AMA 2021 Evaluation and Management Updates

- AMA 2023 Evaluation and Management Updates

- CMS Medicare Claims Processing Manual (Pub. 100-04), chapter 12, section 30.6

- CMS Medicare Program Integrity Manual (Pub. 100-08), chapter 3, section 3.3.2.4 – Signature Requirements

- CMS MLN Fact Sheet, Complying with Medicare Signature Requirements

- Signatures
- Signature Tips


