Reopenings Adjustment Request Form (GRF 679)
Form GRF 679![]() (Reopenings Adjustment Request Form) will allow you to make simple corrections to a previously processed claim. This form may be used if there is no other form to complete the type of correction needed.
(Reopenings Adjustment Request Form) will allow you to make simple corrections to a previously processed claim. This form may be used if there is no other form to complete the type of correction needed.
Requests submitted on GRF 679 are manually processed (non-automated) and may take up to 60 days to complete. Requests to cancel an entire claim or a specific line of a claim may be automated if you submit them using the myCGS® Web Portal.
Only one claim can be corrected per form.
NOTE: In order to complete the form accurately, you must have access to your Remittance Advice (RA). If you download your RA from a billing service or clearinghouse, the line items may be in a different sequence, which will affect the processing on this form. We suggest accessing your RA directly from the myCGS® Web Portal.
Also, to avoid issues with legibility, we encourage you to complete the form online, and then print it.
Automated Reopenings Adjustment Request Form Instructions
- Complete the Header of the form:
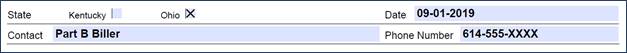
- Select the State
- Enter the date the form is completed
- Enter a contact person's name and telephone number
- NOTE: This information is important should we need to contact you with a question regarding your Reopening request.
- NOTE: This information is important should we need to contact you with a question regarding your Reopening request.
- Complete the Provider Information section:
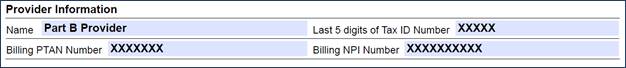
- Identify the last 5 digits of Tax ID number
- Enter the Billing PTAN
- Individual physicians/practitioners who reassign benefits to a group, enter the Group PTAN.
- Solo physicians/practitioners, enter the Individual PTAN.
- Enter the Billing NPI
- Individual physicians/practitioners who reassign benefits to a group, enter the Group NPI.
- Solo physicians/practitioners, enter the Individual NPI.
- Complete the Beneficiary Information section:
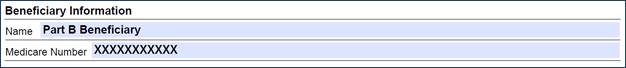
- Enter the Beneficiary's Name
- Enter the Beneficiary's Medicare ID
- To avoid processing delays, please verify that the Medicare ID is correct.
- To avoid processing delays, please verify that the Medicare ID is correct.
- Identify the claim information:
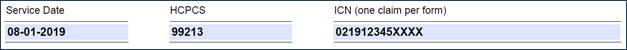
- Enter a Date of Service from the claim.
- Identify a HCPCS/CPT code (procedure code) that corresponds to the date of service.
- Enter the Internal Control Number (ICN) of the claim, which is located on the RA.
- Verify that the ICN is accurate. Incorrect, incomplete, or invalid ICNs will result in increased processing time (up to 60 days).
- Verify that the ICN is accurate. Incorrect, incomplete, or invalid ICNs will result in increased processing time (up to 60 days).
- Complete the Adjustment Details section:
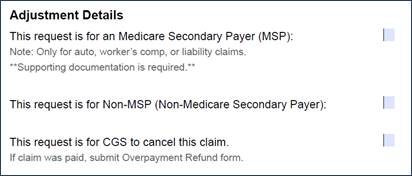
- Check the appropriate box:
- Select Medicare Secondary Payer (MSP) for requests involving auto, Worker's Comp, or liability claims.
- Select Non-MSP for all other requests.
- To cancel an entire claim, select the Cancel this Claim option.
- If the claim was paid, please include a copy of the Voluntary Overpayment Refund Form
 .
.
- Check the appropriate box:
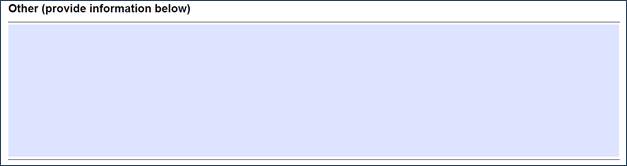
- Provide details about your request in the Other section.
- Please be sure to fully and clearly explain the purpose of the Reopening. For example, explain why your timely filing denial should be adjusted. Do you have an exception to a global surgery denial you received? Explain it in this section.
- Verify your request is an actual REOPENING and opposed to a REDETERMINATION. For example, do you need to correct a diagnosis code and have medical documentation to support the correction? Submit this as a REDETERMINATION, as this situation is not a "simple correction."
- Refer to the Part B Appeals Decision Tree for help determining whether to request a REOPENING or a REDETERMINATION.
- Refer to the Part B Appeals Decision Tree for help determining whether to request a REOPENING or a REDETERMINATION.
- Be sure there is no other Reopenings form specific to your request.
Reopenings request received with invalid or incorrect information will result in the request being returned.

