Top Provider Questions – EDI
Click on an item to expand or Show All / Close All
- I am receiving the following Claim Status Code and EIC code on my 277CA. What do these codes mean?
496-Submitter not approved for electronic claims submission on behalf of this entity.
85-Billing provider-
These messages indicate that you are not set up to bill electronically in the ANSI 5010 format. Please contact the EDI Help Desk prior to moving to production (866-276-9558, option 2).
Reviewed 12/05/2025
-
- I am receiving the following CSC and EIC code on my 277CA. How do I make the correction?
CSC-663 Entity's Group name
CSC-732 Information submitted inconsistent with billing guidelines
EIC IL Subscriber-
The subscriber Group name (SBR04/2000B) element must be empty. The group number (element SBR03/2000B must also be empty.
Reviewed 12/05/2025
-
- I am receiving the following Claim Status Code (CSC) and EIC code on my 277CA. How do I correct this error?
-
CSC-500-Entity's Postal/ZIP code
EIC-77-Service Locations
The service facility location (2310C Claim level) loop requires a 9 digit zip code.Reviewed 12/05/2025
-
- I heard that 5010 requires a physical address in box 33 and P.O. boxes are no longer accepted. Is this true?
-
Yes. 5010 does require a physical address for the billing provider's location (loop 2010AA). Claims received with a P.O. Box in place of a physical address will receive an error and the file will not be accepted into the system.
Reviewed 12/05/2025
-
- I received a payer acknowledgement/Acceptance report from my clearinghouse. Does this mean you accepted my claims?
-
CGS returns back to the submitter, in this case the clearinghouse, a 999 report. If the 999 report was accepted a 277CA report is generated and sent to the submitter. The 277CA report will include ICN/DCN number for accepted claims. Please contact your clearinghouse if you are not receiving these acknowledgement/acceptance reports in a readable format.
Reviewed 12/05/2025
-
- How often is the PC-ACE Pro32 software upgraded?
-
The software is upgraded quarterly. Please visit our website for the latest version. Please note you may only upgrade one version before the current version. Otherwise, you will need to uninstall the old version and then download the full install of the current version.
Reviewed 12/05/2025
-
- I am missing an Electronic Remittance Advise (ERA) or Notice (ERN). How do I order a duplicate?
-
The owner of the submitter ID must make the request. If you go through a clearinghouse that has 1 submitter ID for all their clients the clearinghouse must make the request. You may contact our help desk at 866.276.9558 option 2, or you may visit our website.
Reviewed 12/05/2025
-
- How long are Electronic Remittance Notices (ERN)/Electronic Remittance Advices (ERA) available in my mailbox?
-
Your Electronic Remittance Notices (ERN)/Electronic Remittance Advices (ERA) posted to your mailbox are only available for 14 days. Be sure to download them immediately so reruns and restores are not necessary at the end of the month.
Reviewed 12/05/2025
-
- My claim is rejected with a 306 message on my 277CA. What does this denial indicate?
-
If the procedure is a non-specific code you must submit a description of the procedure code in the SV1 segment, element 01-7. Non-specific codes may include in their descriptors terms such as:
Not Otherwise Classified (NOC); Unlisted; Unspecified; Unclassified; Other; Miscellaneous; Prescription Drug, Generic; or Prescription Drug, Brand Name.
Reviewed 12/05/2025
-
- I received a 277CA report with errors. How can I identify these errors?
-
The 277CA Edit Lookup Tool will allow you to view your errors in easy to understand descriptions.
Reviewed 12/05/2025
-
- Why did CGS return my Online EDI Application for the Provider Authorization Form?
-
It is important that you complete and fill out the Provider Authorization Form after clicking on 'SUBMIT' when doing the online application. The Provider Authorization Form is linked with the actual application it was generated from when the 'SUBMIT APPLICATION' button was depressed. Once you go to the link it has provided you must print out the Provider Authorization Form only, input the TAX ID number and have it signed by an authorized official from the provider. You may not use the same Provider Authorization form for any other applications completed. It will not link to the current one it was generated from. Applications are returned if the Provider Authorization form is not received within seven days.
Reviewed 12/05/2025
-
- I received my application back with errors on my Provider Authorization Form. Can I correct and refax it or will I have to complete an entirely new application and authorization form?
-
Once an application has been processed, if there are any corrections needed, you will have to fill out another EDI Online Application and Provider Authorization Form. We no longer accept corrections. Please refer to the online instructions to ensure you have completed your application thoroughly before submitting.
Reviewed 12/05/2025
-
- I need help understanding the 277CA rejection that I received.
-
The 277CA Edit Lookup Tool allows Trading Partners, billing services, providers, and clearinghouses to view easy-to-understand descriptions associated with the edit code(s) returned on the 277CA – Claim Acknowledgment for 5010A1 claims. The tool allows you to enter the edit codes and will return possible explanations for the cause of the edit.
Step 1: Access the 277CA Edit Lookup Tool
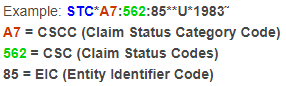
Step 2: Enter the edit information located in the STC segment or reported on your acknowledgment file into the 5010A1 277CA Edit Lookup Tool
Step 3: Click Submit
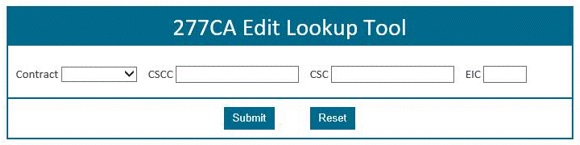
The results will be returned below the search fields and will display all possibilities for the cause of the edit.
For additional instructions, please refer to 277CA EDI Edit User Guide

Reviewed 12/05/2025
-
- How do I verify DDE/PPTN enrollment?
-
Step 1:
Complete the J15 DDE PPTN Application/Reactivation form.
Step 2:
Once submitted a Request ID will be generated.
Step 3
If the user(s) is located outside of the US, please send a copy of the network connectivity diagram to CGS.EDI@cgsadmin.com and include your request ID in the subject line of the email.
Step 4:
J15 EDI will complete the DDE PPTN enrollment process within 7 business days.
Step 5:
A confirmation email will be sent to the EDI contact on the application.
Step 6:
If you do not receive a confirmation email, please reach out to the Help Desk at:
Ohio/Kentucky Part B – 1.866.276.9558 (option 2)
Ohio/Kentucky Part A – 1.866.590.6703 (option 2)
Home Health/Hospice – 1.877.299.4500 (option 2)Reviewed 12/05/2025
-

