Cardiac Rehab with Continuous ECG Monitoring ADR Checklist
CGS recommends providers organize the medical documentation in the order indicated below. This will assist CGS in reviewing your documentation more efficiently, and will expedite the review process. Please ensure the documentation is submitted within 45 days of the Additional Documentation Request (ADR). If the documentation has not been received, the claim will automatically deny on the 46th day for non-receipt of documentation.
Providers should submit all documentation that is pertinent to support the medical necessity of services for the billing period being reviewed. Ensure services billed are coded accurately for the service provided and the documentation supports those services. This may include documentation that is prior to the review period, such as an Individualized Treatment Plan (ITP). Please note that the most common reason for overturned appeals are due to providers submitting new documentation upon the appeal that was omitted with the initial submission of medical records.
*Please include the beneficiary name and date of service on all documentation and include an abbreviation key (if applicable). Documentation must be legible and complete (including signature(s) and date(s)). If you question the legibility of your signature, you may submit a signature log or an attestation statement.
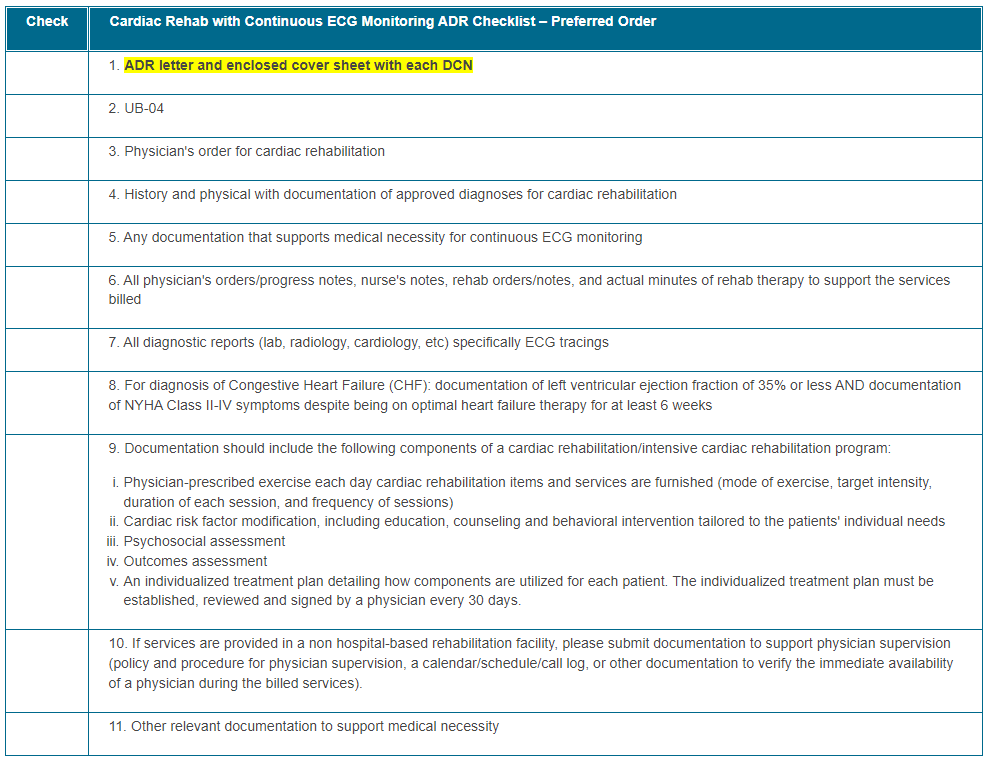
The Checklist below is intended to be utilized by providers as a reference when responding to Additional Documentation Requests (ADR) to ensure each claim meets the policy requirements prior to the ADR submission. Please submit all documentation as required in the LCD or NCD if applicable and in accordance with the Medicare Benefit Policy Manual. It is the responsibility of the provider to submit complete and accurate documentation per the regulatory guidelines for each claim. Ensure the documentation submitted belongs solely to the intended beneficiary and documentation of another beneficiary is not present within any aspect of the medical record.
Click on the table below for a printable version.
Helpful Links:
- Medicare Benefit Policy Manual 100-2, Chapter 15 Section 232

- Cardiac Rehabilitation: Coverage and Documentation Requirements
- Electronic Code of Federal Regulations §410.49

- Signature Requirements: CMS Medicare Program Integrity Manual: (page 43) (Pub. 100-08), Chapter 3, Section 3.3.2.4

How to Prevent Common Denials
Ensure Documentation includes:
Medicare covers cardiac rehabilitation services for beneficiaries who have experienced one or more of the following:
- An acute myocardial infarction (MI) within the preceding 12 months (the date patient had the MI must be documented in the records)
- A coronary bypass surgery; (Send OP Report)
- Current stable angina pectoris (Cardiologist office visit note, progress note, or other documenting stable diagnosis.
- Heart valve repair or replacement; (Send OP Report)
- Percutaneous transluminal coronary angioplasty (PTCA) or coronary stenting; (Send OP Report)
- A heart or heart-lung transplant (Send OP Report)
- Stable, chronic heart failure: (2 components must be supported)
- Left ventricular Ejection fraction of 35% or less
- New York Heart Association (NYHA) class II to IV symptoms despite being on optimal heart failure therapy for at least 6 weeks)
- Other cardiac conditions as specified through a national coverage determination (NCD)
- All Cardiac Rehabilitation (CR) Program Component Requirements
Claims must have all 5 components to be paid. Components may be separate or compiled together in the Individualized Treatment Planned (ITP).
- Physician-prescribed exercise each day cardiac rehabilitation items and services are furnished will include:
- Mode of exercise (typically aerobic)
- Target intensity (e.g., a specified percentage of the maximum predicted heart rate, or number of METs)
- Duration of each session (e.g., "31 minutes")
- Frequency (number of sessions per week)
- Coronary risk factor modification (education, behavioral intervention or training tailored to meet the patient's (pt's) individualized needs, including education on cardiac management)
- Education/training should assist in achievement of individual goals towards independence in activities of daily living (ADL), adaptation to limitations, and improved quality of life
- Providing educational pamphlets with no follow up or providing only patient assessments at the beginning and end of the program are not acceptable to support the intervention
- Psychosocial assessment (include screening tool utilized)
- Must be thorough and occur at periodic intervals
- Provide information on the patient's support system, family, how cardiac diagnosis affects their life, counseling, etc. (Psychosocial testing results such as PHQ-9 can be submitted)
- Example: How does the patient view their quality of life and what education is important to them?
- Outcomes assessment (to determine if the interventions did or did not result in some benefit to the pt)
- Provide an ongoing evaluation of the interventions and goals for the patient including results or modifications required
- Example: If weight loss and lowering cholesterol are goals how is that being addressed and how is the pt progressing to meet that goal or not?
- Provide an ongoing evaluation of the interventions and goals for the patient including results or modifications required
- Individualized Treatment Planned (ITP) established, reviewed, signed and dated by physician every 30 days to cover the dates of service (DOS) billed
- This may require submitting the ITP competed prior to the review period
- Example: The DOS billed on the claim – 11/04/22, 11/06/22, 11/08/22, 11/14/22, 11/25/22 and 11/29/22. The ITP submitted is dated 11/25/22. This only covers DOS 11/25/22 and 11/29/22 for this claim (the ITP dated 11/25/22 is valid until 12/25/22, 30 days). This will result in a partial denial unless the previous ITP completed is submitted to cover all the DOS billed. The ITP dated 10/25/22 must be submitted as well to cover the 11/04/22, 11/06/22, 11/08/22, and 11/14/22 DOS billed. (the ITP dated 10/25/22 is valid until 11/25/22, 30 days).
- Clear documentation of total session minutes and ECG Tracings provided for each DOS billed
- 1 billed session must be at least 31 minutes and 2 billed sessions must be at least 91 minutes.
- Sessions are limited to a maximum of 2 1-hour sessions per day for up to 36 sessions over up to 36 weeks with the option for an additional 36 sessions over an extended period of time, if approved by CGS.
- If the sessions exceed 36 sessions and are not billed with the KX modifier, services will be denied.
- Physician order for cardiac rehabilitation signed legibly and dated. If the physician's signature is not signed electronically, the physician's 'NAME' and Credentials must be PRINTED on the order. A signature log or attestation statement may be submitted. If the signature is illegible and the name is not printed, the claim will be denied.
- History and physical exam, cardiac catheterization reports, cardiac operative reports, cardiology office note(s) or other provider note(s) which include information supporting the diagnosis and treatment. Diagnostic reports (lab, radiology, cardiology, etc) to help support diagnosis.
Please contact J15AMREDUCATION@cgsadmin.com for further questions, concerns,or educational needs related to the TPE process. Be sure to include the facility name and Provider number/PTAN for the inquiry. Ensure CGS is current with provider contact information for any educational outreach opportunity.
Updated: 08.20.2025