Top Provider Questions – EDI
Click on an item to expand or Show All / Close All
- I need help understanding the 277CA rejection that I received.
-
The 277CA Edit Lookup Tool allows Trading Partners, billing services, providers, and clearinghouses to view easy-to-understand descriptions associated with the edit code(s) returned on the 277CA – Claim Acknowledgment for 5010A1 claims. The tool allows you to enter the edit codes and will return possible explanations for the cause of the edit.
Step 1: Access the 277CA Edit Lookup Tool
Step 2: Enter the edit information located in the STC segment or reported on your acknowledgment file into the 5010A1 277CA Edit Lookup Tool
Step 3: Click Submit
Example: STC*A7:562:85**U*1983˜
A7 = CSCC (Claim Status Category Code)
562 = CSC (Claim Status Codes)
85 = EIC (Entity Identifier Code)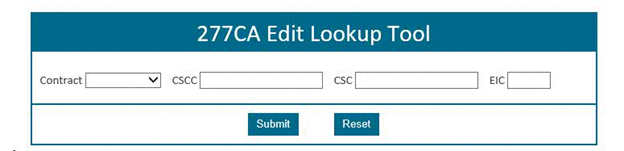
The results will be returned below the search fields and will display all possibilities for the cause of the edit.
For additional instructions, please refer to 277CA EDI Edit User Guide
Reviewed 11/22/2021
-
- How do I verify DDE/PPTN enrollment?
-
- Step 1:
-
Complete the J15 DDE PPTN Application/Reactivation
 form.
form. - Step 2:
-
Fax in the completed application. The Fax numbers are located on the bottom of the form.
- Step 3:
-
J15 EDI will complete the DDE PPTN enrollment process within 20 business days.
- Step 4:
-
A confirmation e-mail will be sent to the EDI contact on the application
- Step 5:
-
If you do not receive a confirmation email, please reach out to the Help Desk at:
Ohio/Kentucky Part B – 1.866.276.9558 (option 2)
Ohio/Kentucky Part A – 1.866.590.6703 (option 2)
Home Health/Hospice – 1.877.299.4500 (option 2)
Reviewed 11/22/2021
-
- What is the status of my EDI Application?
-
Our EDI department has seen an increase in status calls on the EDI applications. All application confirmation letters are sent to the correspondence/contact address listed on the original application that was submitted to EDI. Please reach out to this address to locate your letters and the status of your response. Check out our status checker to obtain the current status of your EDI application.
Reviewed 09/22/2021
-
- My DDE password needs to be reset; whom should I contact?
-
If you need to have your DDE User ID password reset, please contact the CGS Security Administration Team at 615.660.5444. Please have the following information ready before calling:
User ID
First and last name of the user to which that ID is assigned
Provider Transaction Access Number (PTAN), if available
Error messageNote: Be sure to change your password every 29 days to avoid having to have it reset.
Reviewed 11/22/2021
-
- When completing the J15 DDE PPTN Application/Reactivation form, do I need to include my current User ID or any previous User IDs I have had?
-
Yes. Submitting this information on the form will assist CGS in determining whether we need to assign you a new user ID.
Reviewed 09/22/2021
-
- Will I be able to obtain Electronic Remittance Advices (ERAs) for checks that were issued prior to my setup?
-
ERA becomes effective the day we complete your setup in our system. You will not be able to access remittances electronically that were issued prior to completion of your setup. Remits issued prior to the set up date may be available through myCGS® or the CGS Part A IVR.
Reviewed 09/22/2021
-
- I am receiving the following Claim Status Code and EIC code on my 277CA. How do I correct this error?
CSC – 500 Entity's Postal/ZIP code
EIC – 77 Service Locations-
Ensure that you are using a valid 9-digit ZIP code for the service facility location (2310E Claim level).
Reviewed 09/22/2021
-
- I am receiving the following Claim Status Code and EIC Code on my 277CA. What do these codes mean?
496 – Submitter not approved for electronic claims submissions on behalf of this entity
85 - Billing provider-
These messages indicate that you are not set up to bill electronically in the ANIS 5010 format. Please contact the EDI Help Desk prior to moving to production (866.590.6703, option 2).
Reviewed 09/22/2021
-
- My claim is rejecting with a 306 message on my 277CA report. What corrections do I need to make to my claim?
306 – Detailed description of service-
If the procedure is a non-specific code (e.g., a "not otherwise classified" (NOC) code), submit a description of the service in SV202-7. Other phrases that indicate non-specific codes are:
- Unlisted
- Unspecified
- Unclassified
- Other
- Miscellaneous
- Prescription Drug, Generic
- Prescription Drug, Brand Name
Reviewed 09/22/2021
-
- I sent in a 5010 claim file and I have not received my 277CA report. Is something wrong with my claim file?
-
Your file may have rejected on the 999 Functional Acknowledgment. If your file rejected on the 999 report, you will not receive a 277CA. Check the IK5 and IK9 segments of the 999:
Rejected File: IK5*R*5 (5 = one or more segments in error) Â IK9*R This transaction will NOT be forwarded for further processing. Correct the errors, then resubmit the file.
Accepted file: IK5*A Â IK9*A This transaction will be forwarded for further processing and a 277CA will be generated.
For more information on how to read the 999, please refer to the CGS 5010 job aid .
.Reviewed 09/22/2021
-
- I received a payer acknowledgement/Acceptance report from my clearinghouse. Does this mean you accepted my claims?
-
CGS returns back to the submitter a 999 report, and if the 999 was accepted, a 277CA report is generated. The 277CA report will include ICN/DCN number for accepted claims. Please contact your clearinghouse if you are not receiving these acknowledgement/acceptance reports in a readable format.
Reviewed 09/22/2021
-
- Once I submit a 5010 837 claim file, how long should it take to get a 999 and/or 277CA?
-
This process can take from one hour up to 48 hours.
Reviewed 09/22/2021
-
- How often is PC-ACE Pro32 software updated?
-
The software is updated quarterly. Please visit our website for the latest version. Please note: you may only upgrade one version before the current version.
Reviewed 09/22/2021
-
- I am missing an Electronic Remittance Advice (ERA). How do I request a duplicate?
-
The owner of the submitter ID must make the request. If you go through a clearinghouse that has 1 submitter ID for all their clients, the clearinghouse must make the request. ERAs older than 45 days cannot be restored electronically. You may also access remits through my CGS, and you may obtain paper copies through the IVR.
Reviewed 09/22/2021
-
- I am receiving the following CSC and EIC Code on my 277CA. How do I make the correction?
CSC- 663- Entity's Group Name
CSC- 732- Information submitted inconsistent with billing guidelines
EIC- Subscriber-
The subscriber Group Name (SBR04/2000B) element must be empty. The group number (element SBR03/2000B) must also be empty.
Reviewed 09/22/2021
-
- We have multiple providers with multiple NPIs. All of our EDI transactions are submitted through one submitter ID. Can we receive a separate 835 ERA for each NPI, and if so, how do we accomplish this?
-
If each NPI has an assigned PTAN, you can receive a separate ERA for each NPI. If you are not using a clearinghouse to receive ERAs, follow these steps:
- Fill out an EDI application indicating that you are requesting a new submitter ID and click submit. (The system will then direct you to the provider authorization form). The online form and other agreement information is available on the CGS website.
- Fax the provider authorization form.
- Repeat Steps 1 & 2 for each PTAN/NPI combination
Note: it may take up to 7 calendar days to process each application. Please fax all applications at the same time. The above option will create multiple submitter IDs, but you will receive separate ERAs for each NPI.
Reviewed 09/22/2021
-
- How do we get AARP co-insurance to cross over to Medicare? Is there a problem with that for CGS?
-
AARP is a supplemental insurance and may pay secondary to (after) Medicare. Here is how the crossover process works: an eligibility file is sent from the Trading Partner (supplemental insurance company) to the BCRC. The file contains data to identify the Medicare Identifier number and claims criteria, specified by the Trading Partner, for crossovers. Each Trading Partner is issued a COBA ID. The COBA ID and eligibility file data, along with information specific to that trading partner, are stored in Medicare's Common Working File (CWF). When claims are processed, CWF compares each COB trading partner's claims selection criteria against the Medicare claims. If the claim matches the Trading Partner's claims criteria and HICN in the trading partner's eligibility file, the claim information is automatically, electronically forwarded to the Trading Partner.
Reviewed 09/22/2021
-
- Our remit area has a few concerns when contacting CGS for missing remits. When we call about a missing remit, they normally want to restore an entire day's file without confirming if one check number was actually present within the file to be restored. What do we need to provide to make sure that we are getting the correct information?
-
Some files submitted, especially by your Clearinghouse or Billing Entity have thousands of claims within the file, this would be a lengthy process for our EDI Help Desk Representatives to look for one remit.
Another alternative would be to register for myCGS® which gives you the opportunity to view each remit separately.
We recommend that you have the following information available when you contact the EDI Help Desk Desk at 866.590.6703 (Option 2) to have remits restored:
- PTAN
- NPI
- Last 5 digits of your Tax ID
- Check/EFT number
- Check/Remittance Date
- Check Amount
Reviewed 09/22/2021
-
- Where can I go to get a correct remit? Do the EDI Help Desk representatives have access to confirm whether a certain check was present?
-
First and second level EDI analysts have access to view certain check/remit information. They can assist providers with check/remit information as long as the provider is able to share valid information (PTAN, NPI and last 5 digits of Tax ID)
Additionally, by registering for myCGS® you would have instant access to view all of your remits.
Reviewed 09/22/2021
-
- How do I sign up for Direct Data Entry?
-
Sign up through the CGS website. From the website, select EDI from the left side of the page and select the EDI Enrollment Packet link. Should you need assistance completing the J15 DDE PPTN Application/Reactivation
 for DDE, call 866.590.6703 (select Option 2).
for DDE, call 866.590.6703 (select Option 2).Reviewed 09/22/2021
-
- I received a 277CA report with errors. How can I identify these errors?
-
The 277CA Edit look-up tool will allow you to view your errors in easy to understand descriptions.
Reviewed 09/22/2021
-
- Do I have recertify my DDE user ID?
-
Each year, Medicare providers are required to recertify their Fiscal Intermediary Standard System (FISS) Direct Data Entry (DDE) user access. You must verify all User IDs, sign, and date the Annual DDE PPTN Recertification Form
 at the bottom. Notification for DDE recertification is sent out via listserv.
at the bottom. Notification for DDE recertification is sent out via listserv.Reviewed 09/22/2021
-
- Why is CGS accepting only the Online EDI Application and EDI Enrollment Agreement From?
-
To ensure the CGS EDI department receives accurate and legible information with form submittals, EDI forms transitioned to a paperless environment. All EDI enrollment forms including EDI Enrollment Agreement and the EDI application form are required to be completed and submitted online beginning May 1, 2020
Reviewed 09/22/2021
-
- Why did CGS return my Online EDI Application for the Provider Authorization Form?
-
It is important that you complete and fill out the Provider Authorization Form after clicking on 'SUBMIT' when doing the online application. The Provider Authorization Form is linked with the actual application it was generated from when the 'SUBMIT APPLICATION' button was depressed. Once you go to the link it has provided you must printout the Provider Authorization Form only, input the TAX ID number, and have it signed by an authorized official from the provider. You may not use the same Provider Authorization form for any other applications completed. It will not link to the current one it was generated from. Applications are returned if the Provider Authorization form is not received within seven days.
Reviewed 09/22/2021
-
- I received my application back with errors on my Provider Authorization Form. Can I correct and refax it or will I have to complete an entirely new application and authorization form?
-
Once an application has been processed, if there are any corrections needed, you will have to fill out another EDI Online Application and Provider Authorization Form. We no longer accept corrections. Please refer to the online instructions to ensure you have completed your application thoroughly before submitting.
Reviewed 09/22/2021
-

