Medical Review Additional Documentation Request (ADR) Process: Prepayment Review
WHAT IS AN MR ADR? – When a claim is selected for medical review, a medical review additional documentation request (MR ADR) is generated requesting medical documentation be submitted to ensure payment is appropriate. Documentation must be received by CGS within 45 calendar days for review and payment determination.
WHY AN MR ADR? – Any claim submitted to CGS may be selected for medical review and generate an MR ADR. Claims may be selected when elements on the claim match the parameters of a prepayment edit established by CGS. A current list of prepayment edits can be accessed on the Home Health and Hospice Medical Review Activity Log.
The information below will help ensure that necessary steps are taken to submit documentation timely and avoid claim denials as a result of the MR ADR process.
- Checking for MR ADRs using FISS
- Using the myCGS® MR Dashboard to Check for MR ADRs and Submit Documentation
- Preparing Your Documentation
- Submitting Your Documentation
- Receipt of Documentation
- Review of Documentation
- ADR Outcomes
- ADR Resources
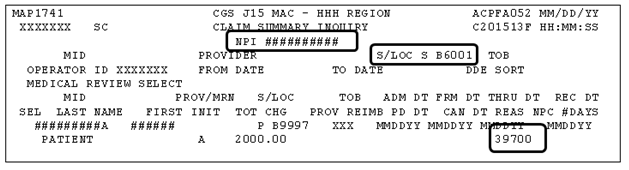
CHECKING FOR MR ADRs USING FISS – When a claim is selected for an MR ADR, the claim is moved to a Fiscal Intermediary Standard System (FISS) status/location S B6001. Providers are encouraged to use FISS Option 12 (Claim Inquiry) to check for ADRs at least once per week.
Your agency should have an internal process established to monitor claims selected for an ADR, and to ensure the documentation is submitted within the required timeframe. If the requested documentation is not received timely by CGS, the claim will be automatically denied.
To check for MR ADRs using FISS Option 12, key your NPI number, the status/location 'S B6001', and press Enter. Claims selected for MR ADR will appear with reason code 39700.
FISS Pages 07 and 08 — Each claim that appears in S B6001 must be selected to identify the documentation that is being requested, as well as the timeframe by which the documentation must be received. This information is found on FISS Pages 07 and 08. These pages only appear when the claim is in status/location S B6001. Screen print FISS pages 07 and 08 for your reference. CGS requires FISS Page 07 be returned with the ADR documentation.
FISS page 07 includes the:
- Patient's Medicare ID;
- Claim dates of service;
- Claim document control number (DCN);
- Mailing address to which your documentation must be sent;
- "Due Date", which is the 45th day. The requested documentation must be received by CGS on/before 45 calendar days of the request. According to the CMS Pub. 100-08, Ch. 3 §3.2.3.2
 ), claims will be denied if the documentation is not received by day 46. Refer to the Additional Documentation Request Timeliness Calculator for assistance in determining the date ADR documentation must be received.
), claims will be denied if the documentation is not received by day 46. Refer to the Additional Documentation Request Timeliness Calculator for assistance in determining the date ADR documentation must be received.
Example of FISS Page 07:
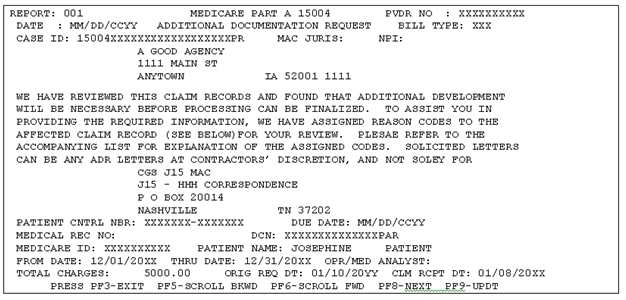
Press F6 to view the entire message. Press F5 to return to the beginning of FISS Page 07.
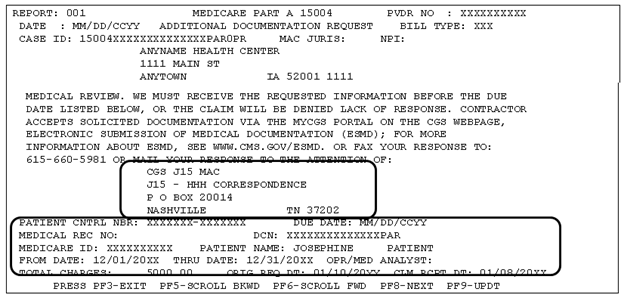
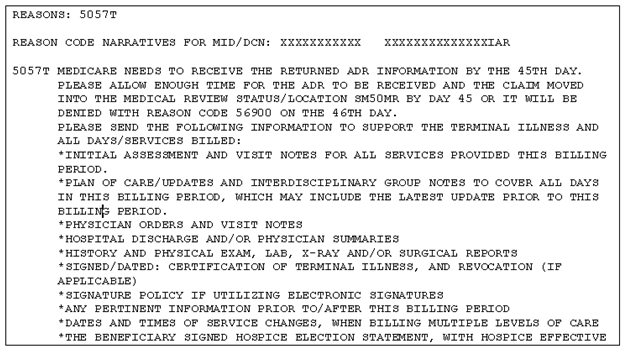
FISS Page 08 is a list of the documentation being requested. This may include initial assessments, the plan of care, physician's orders, visit notes, the certification of terminal illness and election statement (hospice), and OASIS assessments (home health). You may need to press F6 to view the complete list of requested documentation. In addition to the listed documentation, you should send any other documentation that supports payment of the services billed, even if the documentation is before or after the dates of service on the claim, but relevant to the services provided.
Example of FISS Page 08:
USING THE myCGS® DASHBOARD TO CHECK FOR MR ADRs AND SUBMIT DOCUMENTATION
The myCGS® MR Dashboard is another option for you to quickly identify whether you need to respond to medical review (MR) additional documentation requests (ADR). Refer to the myCGS User Manual: Medical Review section for step by step instructions.
When preparing your documentation, attach a copy of the ADR letter (or FISS Page 07) as the first page to ensure the documentation is matched to the appropriate patient and claim.
If you are responding to multiple MR ADR requests, clearly separate the documentation for each claim. Due to CGS's process for imaging documentation, the use of rubber bands or binder clips, or mailing documentation for each claim in separate envelopes, is recommended. Multiple responses sent together, but not separated, may result in the documentation being imaged as one claim. Do not staple documentation.
CGS recommends providers organize the medical documentation in the order indicated below. This will assist CGS in reviewing your documentation more efficiently and will expedite the review process.
Providers should submit the necessary documentation to support the services for the billing period being reviewed. This may include documentation that is prior to the review period, such as admission records, hospice Interdisciplinary Group (IDG) review, etc.
| Hospice ADR Checklist – Preferred Order | Home Health ADR Checklist – Preferred Order |
|---|---|
|
|
Providers may include an outline or cover letter with their documentation. This can be used by CGS Medical Review staff as a roadmap and prove very helpful to highlight key dates or documentation that supports payment of the claim. However, the cover letter cannot be used as documentation, and the documentation must support the contents of the cover letter in order to be useful.
In addition, providers may use brackets, such as [ ] or { }, asterisks (*) or underlined text in the documentation to draw the reviewer's attention to important information. However, notations should not alter, or give the appearance of altering, the documentation. The use of a highlighter is not recommended.
Documentation may be received by CGS either via US Mail, esMD, Fax, myCGS, or on CD/DVD.
Submit your documentation so that it is received by CGS on/before 45 days ("DUE DATE" on FISS Page 07). Ensure that you allow ample time for mailing and processing of the documentation when received. This will prevent the claim from inadvertently denying. Mail to the address that appears on the ADR letter or FISS Page 07:
CGS J15 MAC
J15 – HHH Correspondence
PO Box 20014
Nashville, TN 37202
NOTE: CGS does not recommend sending your documentation overnight via FedEx or UPS. If prompt mailing of your documentation is necessary to meet the due date, CGS recommends overnight delivery via the US Postal Service to the address above. Using myCGS® to submit your documentation is also an option.
myCGS is a free web portal that allows you to submit your ADR documentation directly to CGS and will help to ensure a timely response to an MR ADR. For more information on submitting MR ADR documentation via myCGS, refer to the myCGS User Manual: Forms information and the myCGS MR ADR Job Aid. myCGS® also provides a secure message confirming receipt of the documentation, and a second message confirming it was accepted.
The Electronic Submission of Medical Documentation (esMD) process may be used as an alternative to mailing your documentation. For more information on the esMD process, refer to the CMS esMD![]() Web page.
Web page.
CGS will also accept documentation submitted via Fax (1.615.660.5981).
RECEIPT OF DOCUMENTATION – When your documentation has been received by CGS, the claim is moved from status/location S B6001 to S M50MR for review. Providers can monitor the S M50MR status/location in FISS to verify that their documentation has been received by CGS. Confirmation of receipt is also provided when using myCGS® to submit your documentation.
REVIEW OF DOCUMENTATION – A CGS nurse reviewer will examine the medical records submitted to ensure the technical components (OASIS, certifications, election statement, etc.) are met, and that medical necessity is supported. CGS has 30 days from the date the documentation is received to review the documentation and make a payment determination. For demand denials (condition code 20), CGS has 60 days from the date the documentation is received to review the documentation.
A hierarchy is used to review documentation. This means that documentation is first reviewed for administrative documentation and then medical documentation. Denials are applied according to the hierarchy; however, any additional findings will be addressed in the medical review findings notification.
| Hospice Hierarchy |
Arrow | Home Health Hierarchy |
|---|---|---|
| Valid election statement and addendum(s) (as applicable) | Technical components: OASIS submission, certification/orders, FTF | |
| Technical components: certification statement, FTF if 3rd or later benefit period | Homebound documentation | |
| POC updated every 15 days | Intermittent skilled nursing or therapies | |
| Disease acuity or trajectory supports 6 month prognosis – LCD L34358: "Hospice Determining Terminal Status" | Reasonable and medically necessary skilled service | |
| Non-routine care supported | Use LCD L33942: "Physical Therapy – Home Health" for guidance (when applicable) | |
| Physician visits | OASIS and coding |
During the review, if a signature is found to be missing or illegible, or an electronic signature cannot be authenticated, the claim will be re-ADRd to you in status/location S B6001. Page 08 will show with edit 5ADR2 with a narrative indicating that additional documentation is required to support the signatures. Page 04 (Remarks) will specify the documentation being requested. The additional signature documentation must be received by CGS within 20 calendar days of the request. A screenprint of Page 07 should be attached to the top of the additional documentation and returned to CGS.
ADR OUTCOMES – Possible outcomes of the MR ADR include payment in full (P B9997), partial payment (P B9997), or a full denial (D B9997). Providers are notified of the payment determination via the FISS status/location, as well as their remittance advice. When a claim is denied with reason code 56900, indicating that the medical documentation was not received by CGS, or was not received timely, a "56900 reopening" may be requested within 120 days of denial to have the medical documentation reviewed by the Medical Review department, without utilizing the Medicare Appeals Process. All other denials for which the provider disagrees may be appealed using the Medicare Appeals Process.
- CGS Prepayment Medical Review Additional Documentation Request Quick Resource Tool

- CGS Additional Documentation Request Timeliness Calculator
- CMS Medicare Program Integrity Manual (PIM), CMS Publication 100-08, Chapter 3, Section 3.2.3,
 "Requesting Additional Documentation During Prepayment and Postpayment Review"
"Requesting Additional Documentation During Prepayment and Postpayment Review" - FISS DDE User Manual
- myCGS User Manual
- Top Provider Questions – Additional Documentation Request (ADR)/Medical Review
Updated: 06.17.2025

