June 22, 2021
J15 Post Pay Resumptive Review Status Update 01/01/2021 – 03/31/2021
Beginning August 17, 2020, CMS directed the MACs to resume fee-for-service medical review activities beginning with post payment reviews of items/services provided before March 1, 2020. Items and services are selected based upon high error rates and/or potential overutilization identified through data analysis.
CGS Medical Review is dedicated to the integrity of the Medicare program. CGS welcomes provider inquiries and continues to offer education sessions to ensure providers understand CMS regulations with the goal of successful reviews resulting in claim payment.
Results for service specific post payment reviews are listed below.
Drugs/Biologicals – J0129, J0178, J2507 |
||
|---|---|---|
Service Specific Results |
Kentucky |
Ohio |
Reviews Completed |
43 |
5 |
Claims Allowed |
0 |
1 |
Claims Denied |
43 |
4 |
No Provider Response |
23 |
4 |
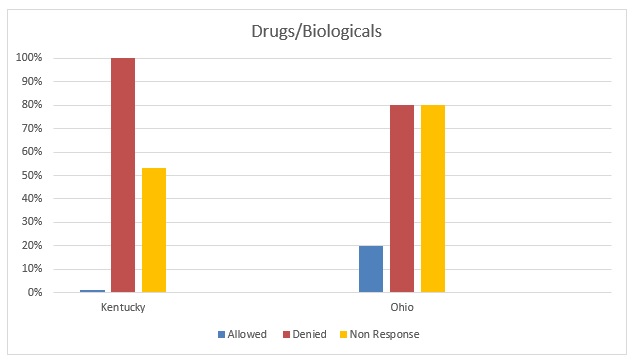
Top Findings:
- The documentation submitted does not support medical necessity. Refer to SSA 1862, IOM, Medicare Program Integrity Manual, Pub 100-08, Chapter 3, Section 3.6.2.1, 3.6.2.2
 .
.
The submitted documentation lacked elements such as orders, purchase orders, patient signed consent, and progress notes supporting the medical necessity of the drug/biological administration. - Non-Response - ADR response should be submitted within 45 calendar days. Claims shall deny as not reasonable and necessary if documentation is not submitted.
SSA 1833(e), IOM, Medicare Program Integrity Manual Pub 100-08, Chapter 3, Section 3.3.2
Social Security ACT – 1833 (e)
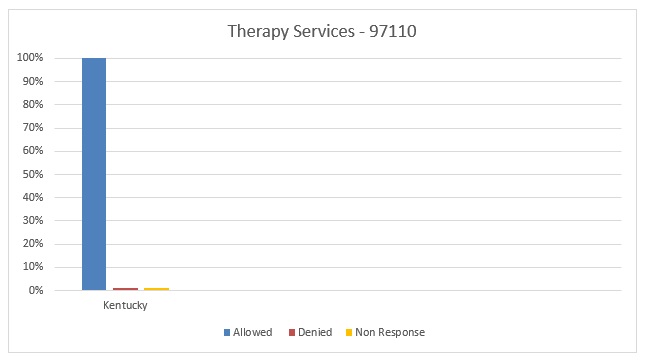
Outpatient Physical and Occupational Therapy Services - 97110 |
||
|---|---|---|
Service Specific Results |
Kentucky |
Ohio |
Reviews Completed |
1 |
0 |
Claims Allowed |
1 |
0 |
Claims Denied |
0 |
0 |
No Provider Response |
0 |
0 |
Importance of responding to Additional Request Documentation:
During postpayment review, there has been a high error rate due to non response to the ADR.
Any claim submitted to CGS may be selected for medical review and generate an MR ADR. When a claim is selected for medical review, a medical review additional development request (MR ADR) is generated requesting medical documentation be submitted to ensure payment is appropriate
- Claims may be selected when elements on the claim match the parameters of a postpayment edit established by CGS.
- Documentation must be received by CGS within 45 calendar days for review and payment determination.
Contractors are authorized to collect medical documentation by the Social Security Act. Section 1833(e) states, “No payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period.”
Section 1815(a) states “….no such payments shall be made to any provider unless it has furnished such information as the Secretary may request in order to determine the amounts due such provider under this part for the period with respect to which the amounts are being paid or any prior period.”
Additional Documentation Requests (ADRs): How and What to Send
New Additional Development Request Timeliness Calculator Self-Service Option
Methods of Responding to ADRs:
ADRs may be submitted via
- Mail: Hardcopy or CD/DVD
- Fax
- myCGS (Free web portal, will accept response to ADRs)
Resources:
- HCPCS J0129 Fact Sheet

- HCPCS J0178 Fact Sheet

- HCPCS J2507 Fact Sheet

- Outpatient Physical and Occupational Therapy Services (LCD L34049) Fact Sheet

- Signature Tips

- CGS Part B MR Activities
Provider inquiries and education requests may be email to J15BMREDUCATION@cgsadmin.com.
CGS encourages providers to request education and conduct self-monitoring based on our posted Medical Review activity log and by using tools such as Comparative Billing Reports (CBRs) offered through our web portal.
To learn more about the post payment resumptive process, please refer to the following links:

