July 7, 2020
New Provider Tips – Medicare Part C and D Eligibility
For providers new to Medicare, please read the tips below to help with your questions on checking Medicare Part C and D eligibility through myCGS®.
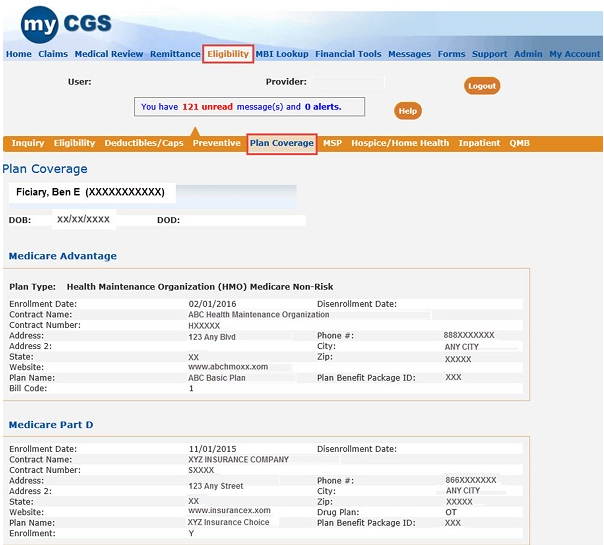
The Plan Coverage tab provides information regarding the beneficiary's enrollment under Medicare Advantage (MA) and Part D contracts and/or MA Managed Care Plans (Part C contracts) that provide Part A and B benefits for beneficiaries enrolled under a contract.
When retrieving the MA Plan or Part D information, myCGS® may provide the following for these contracts:
- Plan Type
- Enrollment Date
- Disenrollment Date
- Contract Number or Plan Benefit Package ID
- Plan Name
- Address
- Phone Number
Please note, when myCGS® indicates that a beneficiary has coverage through a non-Medicare entity (MA or Medicare Drug Benefit plans) the inquiring provider should always contact the non-Medicare entity for complete beneficiary entitlement information. You may also contact the beneficiary for a copy of that plan's card for your records.
Please refer to the myCGS User Manual![]() be for more eligibility information and further guidance.
be for more eligibility information and further guidance.
Not currently using myCGS? Register TODAY!

