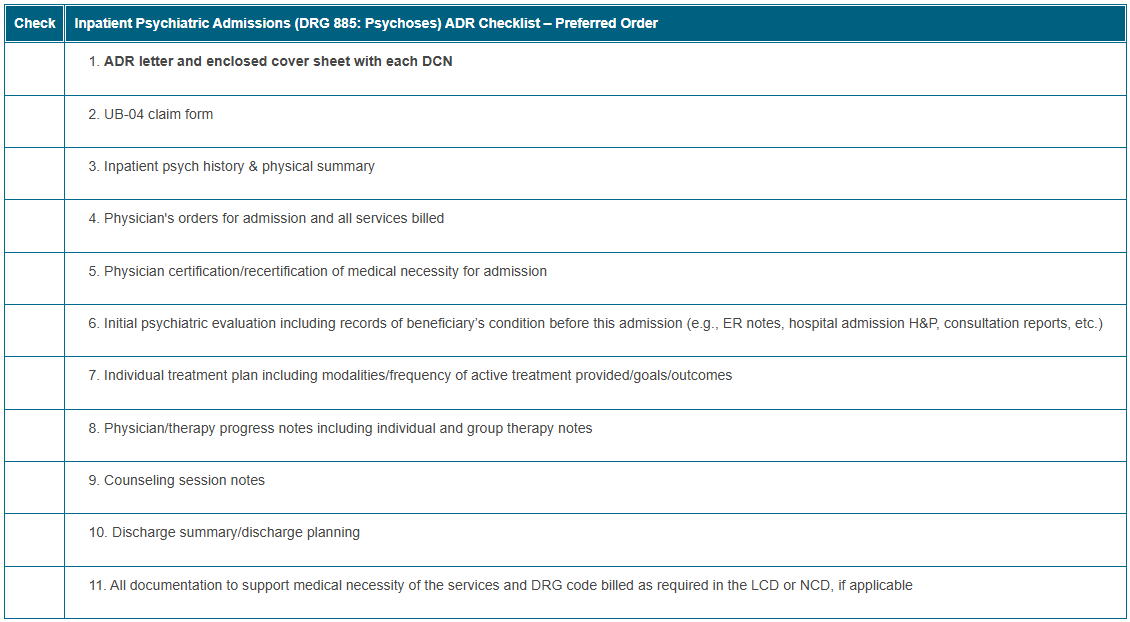
Inpatient Psychiatric Admissions (DRG 885: Psychoses) ADR Checklist
To help us complete a more efficient and expedited review, we recommend organizing medical record documentation in the order indicated in the checklist below. Please ensure you submit the requested documentation within 45 days of the Additional Documentation Request (ADR). If we don’t receive a timely response, your claim will deny for non-receipt of records.
Submit all documentation pertinent to support that the services provided and billed during the review period are medically necessary and coded correctly. This may include documentation for services provided prior to the review period. Please note: The most common reason claim denials are overturned on appeal is because the redetermination (first level appeal) request included new documentation omitted from the initial submission for medical review.
*Please ensure all documentation contains the beneficiary’s name, date of service, and an abbreviation key (if applicable). In addition, all documentation must be complete and legible, including signature(s) and date(s). If the legibility of a signature is questionable, include a signature log or attestation statement.
Before responding to an ADR, use the checklist below as a reference to ensure each claim meets Medicare’s policy requirements. Please submit all required documentation outlined in the CMS Medicare Benefit Policy Manual and any applicable Local Coverage Determination (LCD) or National Coverage Determination (NCD). Providers are responsible for submitting complete and accurate documentation per regulatory guidelines for each claim. Ensure documentation within any aspect of the medical record that you submit belongs solely to the intended beneficiary, and documentation for another beneficiary isn’t present.
Click on the table below for a printable version.
Resources
- CMS Medicare Benefit Policy Manual (Pub. 100-02), Chapter 2

- CMS Medicare Program Integrity Manual (Pub. 100-08), Chapter 3, section 3.3.2.4

- Complying with Medicare Signature Requirements
 MLN fact sheet
MLN fact sheet - ICD-10-CM/PCS MS-DRG v37.2 Definitions Manual

- LCD L34183: Psychiatric Inpatient Hospitalization

- LCD Article A57052: Billing and Coding: Psychiatric Inpatient Hospitalization

- Social Security Act section 1862 (a)(1)(A)
 : definition of “medically necessary”
: definition of “medically necessary”
How to Prevent Common Denials
Ensure documentation includes:
- Physician signed certification or recertification with required components
- If not completed timely, provide a reason for the delay.
- If the physician signature is illegible, provide a signature log or attestation statement.
- Certification is required at the time of admission or as soon thereafter that is reasonable and practicable.
- Recertification is required on the 12th day after admission and no less than every 30 days thereafter.
- Psychiatric evaluation with required components completed within 60 hours of admission
- Progress notes recorded weekly for the first 2 months that contain recommendations for treatment plan revisions
You may include an outline or cover letter with your documentation for CGS Medical Review staff to use as an index and help locate key documentation that supports claim payment. However, the cover letter can’t replace medical record documentation, and the documentation must support the cover letter contents to be useful.
In addition, you may use brackets [ ] or { }, asterisks (*) or underlined text in the documentation to draw the reviewer's attention to important information. However, notations should not alter, or give the appearance of altering, the documentation. Use of a highlighter isn’t recommended since documentation may not be legible.
Education
We encourage all CGS providers to use the myCGS portal. This free self-service option is available 24/7. Registered users can identify and respond to ADRs, determine review status, and receive immediate notifications.
Visit the Calendar of Events to register for our educational sessions.
For any additional questions, concerns, or educational needs related to the TPE process, please email J15AMREDUCATION@cgsadmin.com. Include your facility’s name and provider number (PTAN) with your inquiry. Also, please use this email address to provide current contact information in case CGS identifies any educational outreach opportunity.