Reopenings Reprocess Claim Adjustment Request Form (REP 913)
Form REP 913![]() (Reopenings Reprocess Claim Adjustment Request Form) will allow you to submit a request to reprocess a claim that denied when there are no changes or updates to make to the actual claim. Examples include:
(Reopenings Reprocess Claim Adjustment Request Form) will allow you to submit a request to reprocess a claim that denied when there are no changes or updates to make to the actual claim. Examples include:
NON-MSP
- Update to fee schedule or update to allow new procedure codes.
- Global surgery denials that should be reversed due to an update to a different claim.
- An erroneous duplicate denial. NOTE: Make sure the duplicate denial is incorrect; otherwise the adjustment may result in payment errors and/or recoupments.
MSP
- A patient's file was updated to show Medicare should pay as primary on a claim we originally processed and denied as secondary.
- Includes Medicaid timely filing claims.
Only one claim can be corrected per form.
NOTE: In order to complete the form accurately, you must have access to your Remittance Advice (RA). If you download your RA from a billing service or clearinghouse, the line items may be in a different sequence, which will affect the processing on this form. We suggest accessing your RA directly from the myCGS® Web Portal.
Also, to avoid issues with legibility, we encourage you to complete the form online, and then print it.
Automated Reopenings Reprocess Claim Adjustment Request Form Instructions
- Complete the Header of the form:
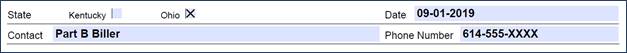
- Select the State
- Enter the date the form is completed
- Enter a contact person's name and telephone number
NOTE: This information is important should we need to contact you with a question regarding your Reopening request.
- Complete the Provider Information section:
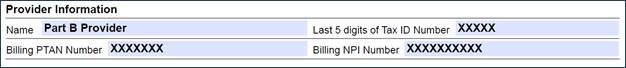
- Identify the last 5 digits of Tax ID number
- Enter the Billing PTAN
- Individual physicians/practitioners who reassign benefits to a group, enter the Group PTAN.
- Solo physicians/practitioners, enter the Individual PTAN.
- Enter the Billing NPI
- Individual physicians/practitioners who reassign benefits to a group, enter the Group NPI.
- Solo physicians/practitioners, enter the Individual NPI.
- Complete the Beneficiary Information section:
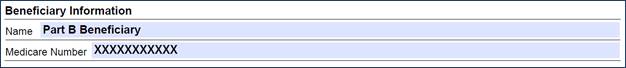
- Enter the Beneficiary's Name
- Enter the Beneficiary's Medicare ID
- To avoid processing delays, please verify that the Medicare ID is correct.
- To avoid processing delays, please verify that the Medicare ID is correct.
- Identify the claim information:
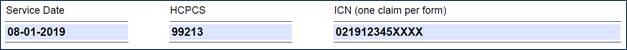
- Enter a Date of Service from the claim.
- Identify a HCPCS/CPT code (procedure code) that corresponds to the date of service.
- Enter the Internal Control Number (ICN) of the claim, which is located on the RA.
- Verify that the ICN is accurate. Incorrect, incomplete, or invalid ICNs will result in increased processing time (up to 60 days).
- Verify that the ICN is accurate. Incorrect, incomplete, or invalid ICNs will result in increased processing time (up to 60 days).
- Complete the Adjustment Details section:
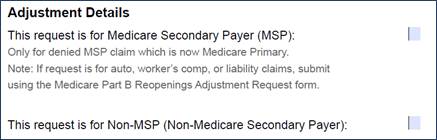
- Check the appropriate box:
- Select Medicare Secondary Payer (MSP) when Medicare is now the primary payer on a claim originally processed as secondary.
- NOTE: Cases involving auto, Worker's Comp, or liability claims must be submitted on the Medicare Part B Reopenings Adjustment Request - GRF 679
 .
.
- NOTE: Cases involving auto, Worker's Comp, or liability claims must be submitted on the Medicare Part B Reopenings Adjustment Request - GRF 679
- Select Non-MSP for all other requests.
- Select Medicare Secondary Payer (MSP) when Medicare is now the primary payer on a claim originally processed as secondary.
- Check the appropriate box:

